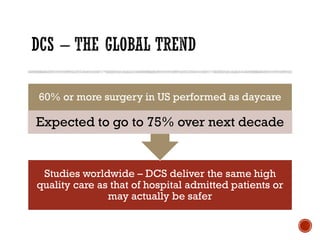
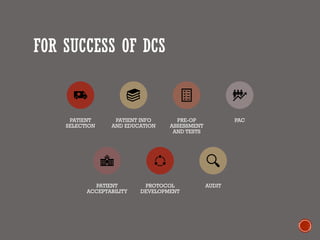
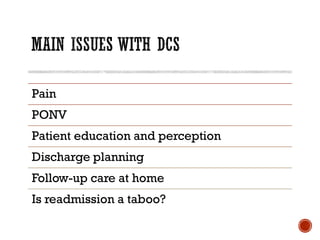
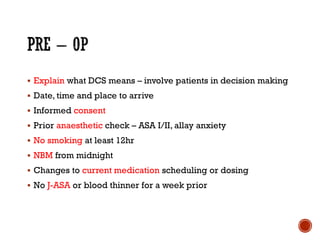
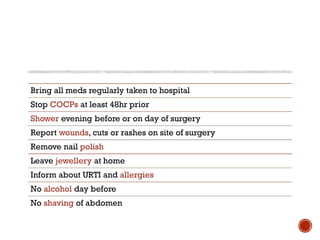
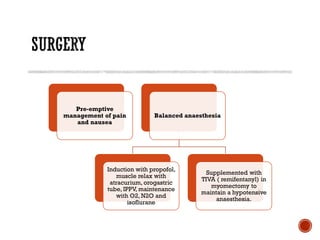
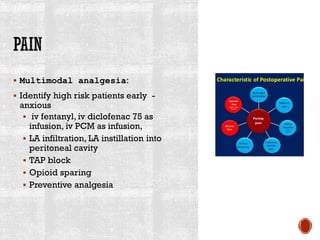
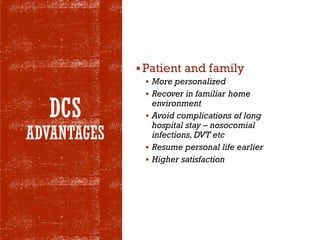
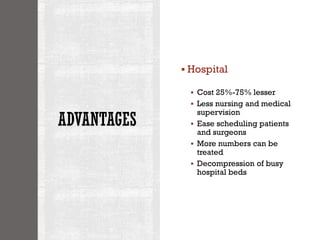
The document presents a comprehensive overview of the evolution and implementation of day care surgery (DCS) in a healthcare setting, highlighting its benefits such as reduced hospital stay, cost savings, and enhanced patient satisfaction. It outlines the criteria for patient selection, surgical procedures performed, and challenges faced in the adoption of DCS, including issues with patient awareness and insurance cooperation. The text also emphasizes the importance of patient education, multimodal pain management, and post-operative care protocols in ensuring successful outcomes for same-day surgeries.

![2011 – 16 cases to 2015 – 489
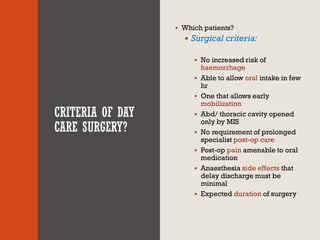
cases
Uterus size – bulky to 28 weeks
Dominant fibroid – 2 to 26.4 cm
Number – 2 to 17
Day care surgery – 456, admissions
33 [7.2%] with only 5[1.1%]
conversions.](https://image.slidesharecdn.com/daycaresurgery2-190718192548/85/Day-care-surgery-9-320.jpg)
![▪ Day care surgery – 365,admissions – 22
[6%]
▪ Uterus size – 40g to 3.27kg
▪ Readmissions, transfers, conversions – None
▪ Blood transfusion – none
▪ Bladder injury – one [0.27%]](https://image.slidesharecdn.com/daycaresurgery2-190718192548/85/Day-care-surgery-10-320.jpg)