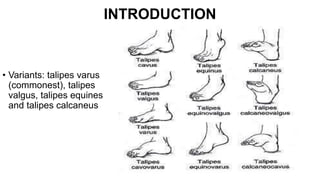
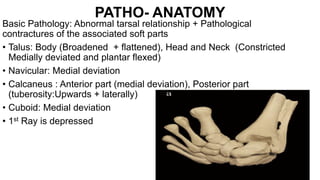
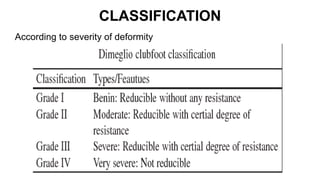
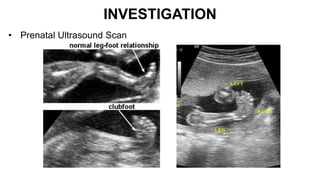
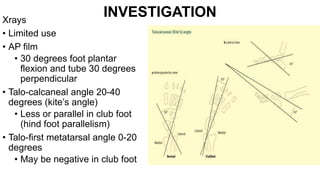
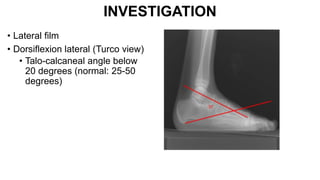
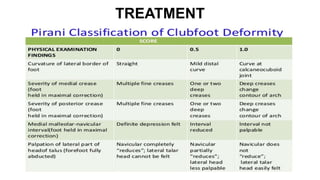
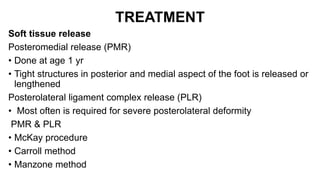
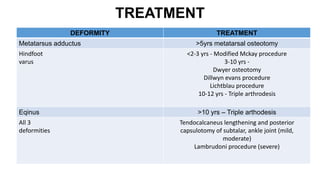
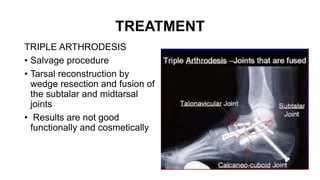
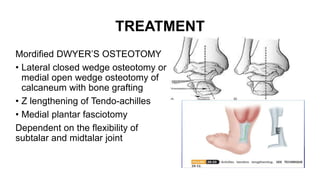
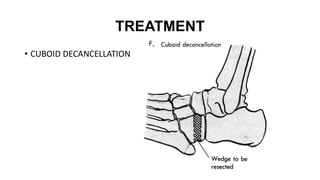
This presentation discusses congenital talipes equinovarus (clubfoot) including its epidemiology, anatomy, classification, clinical features, and management. Clubfoot is a deformity of the foot and ankle characterized by equinus, inversion, adduction and internal tibial torsion. It occurs in approximately 1 in 1000 live births. Treatment involves serial casting or the Ponseti method for mild-moderate cases and soft tissue releases and osteotomies for severe cases. Long term follow up is important to prevent recurrence of the deformity.