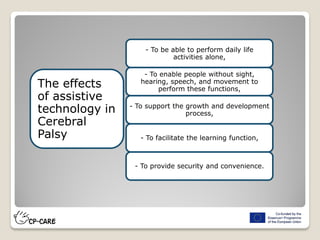
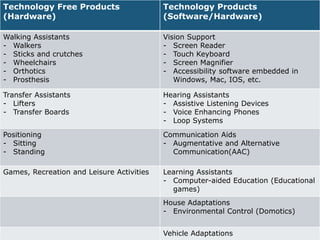
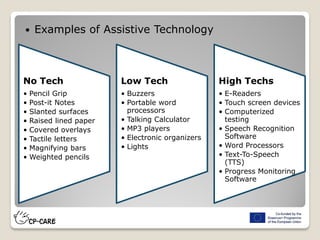
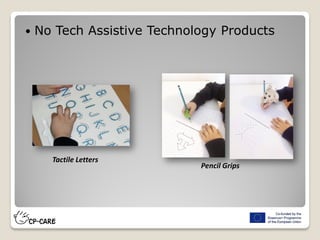
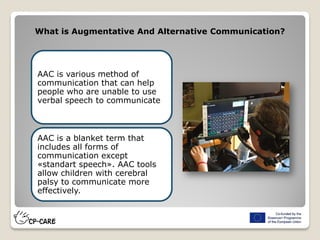
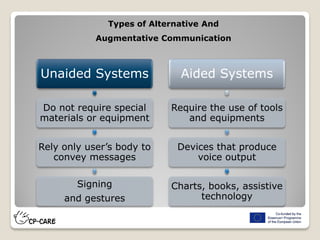
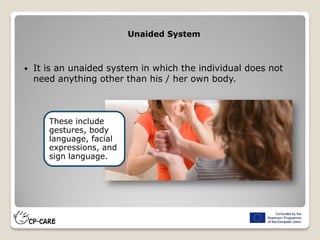
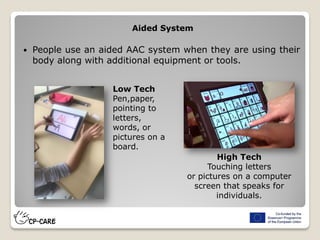
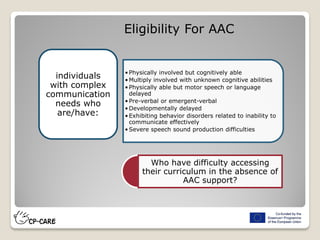
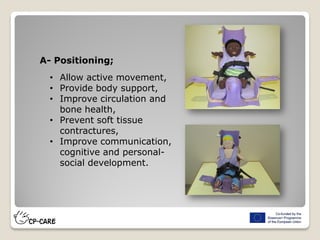
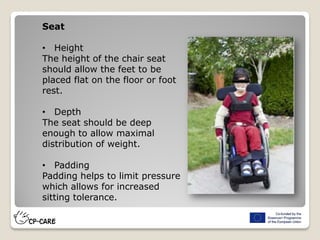
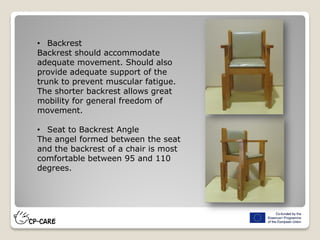
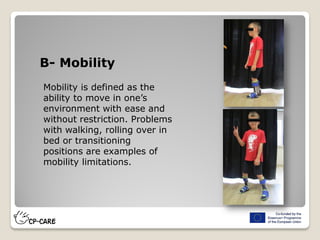
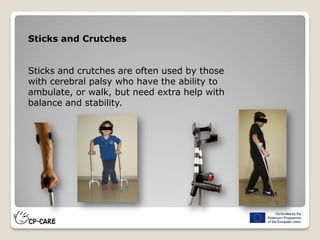
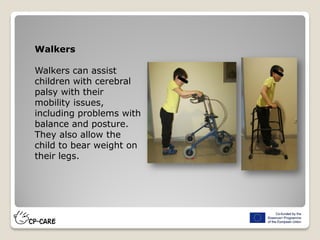
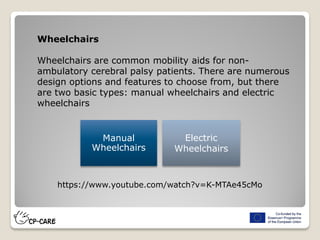
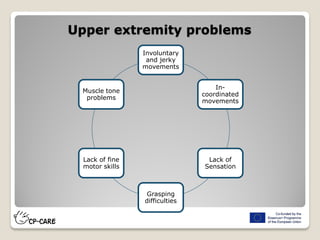
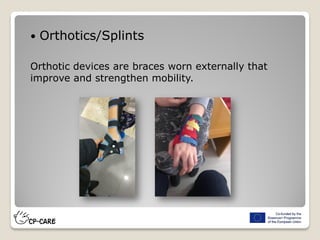
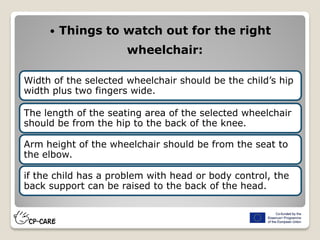
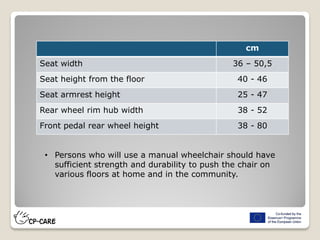
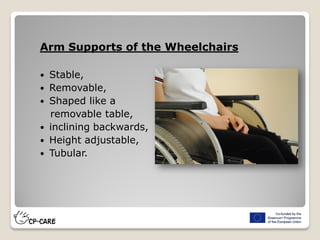
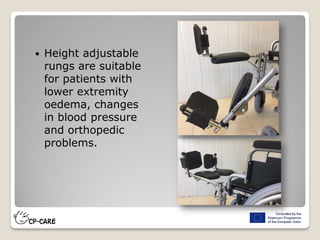
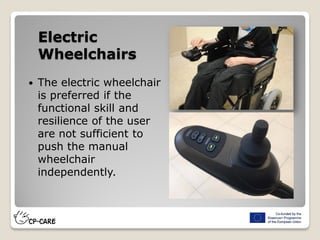
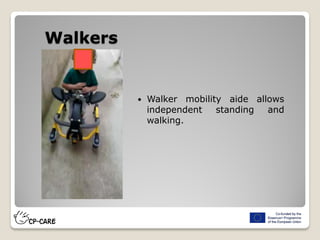
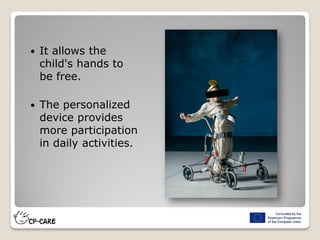
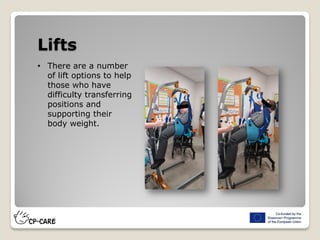
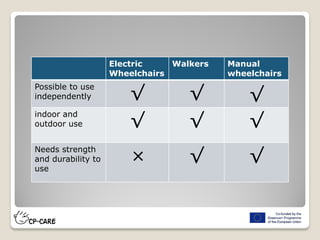
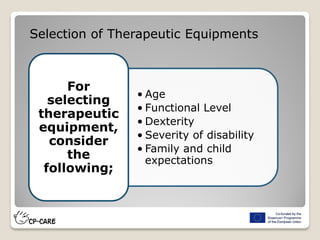
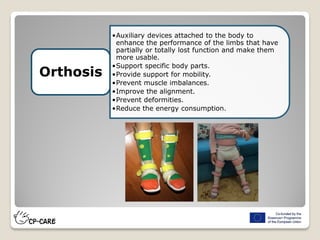
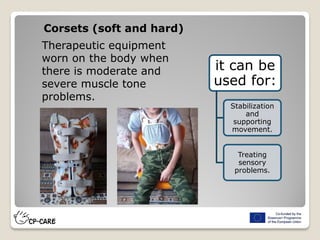
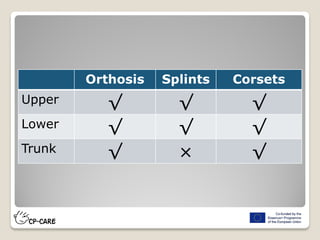
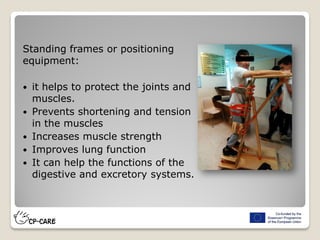
The document discusses assistive technology for individuals with cerebral palsy, detailing various devices and systems that support mobility, communication, and daily activities. It covers categories of technology, including no-tech, low-tech, and high-tech solutions, as well as specific aids for different bodily functions. Additionally, it emphasizes the importance of tailored adaptive equipment to enhance the independence and quality of life for users.