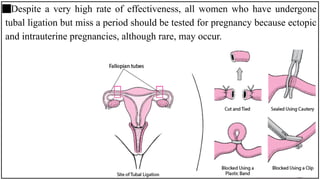
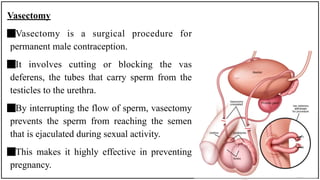
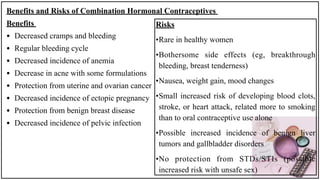
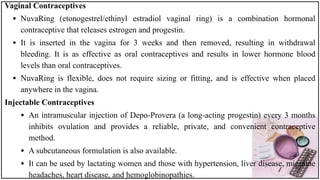
Contraception refers to methods used to prevent pregnancy. There are various contraceptive methods available with different mechanisms and effectiveness rates. Abstinence guarantees 100% effectiveness against pregnancy and STIs but requires strong willpower. Sterilization like tubal ligation and vasectomy are highly effective but permanent. Hormonal methods like oral contraceptives and implants prevent ovulation through hormones while IUDs alter the uterine environment. Each method has advantages and disadvantages to consider.