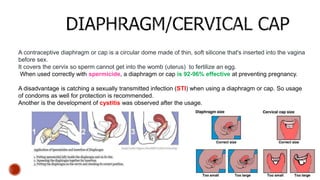
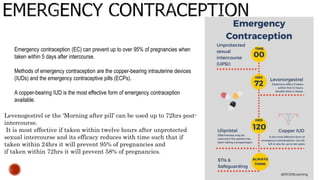
The document provides a comprehensive overview of various contraception methods, including their mechanisms, effectiveness, and potential side effects. It discusses different contraceptives such as condoms, diaphragms, progestin-only pills, birth control injections, and emergency contraception options, detailing their usage and recommendations. Additionally, it outlines specific considerations and contraindications for certain populations, such as postpartum women and those with specific health conditions.