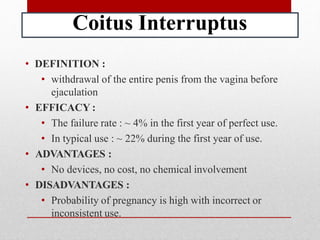
This document summarizes various contraceptive methods. It discusses periodic abstinence methods like coitus interruptus and lactational amenorrhea. It also describes mechanical barriers like condoms, diaphragms and caps. The document outlines several hormonal contraceptives including implants, injectables, pills and patches. It provides details on effectiveness, advantages and disadvantages of each method. The ideal characteristics of contraception are also stated in the beginning.