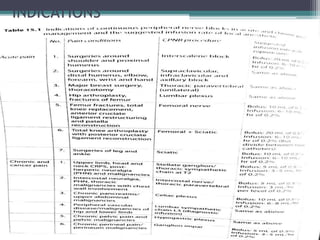
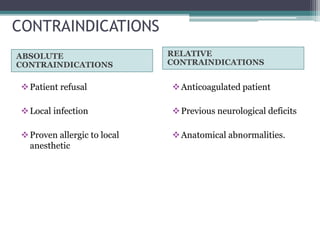
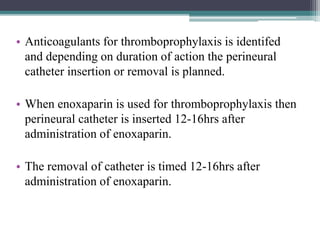
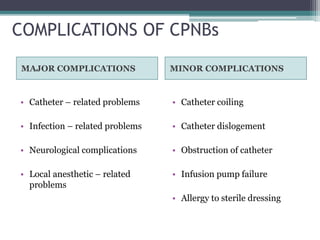
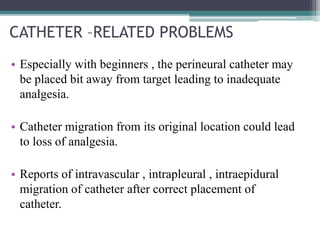
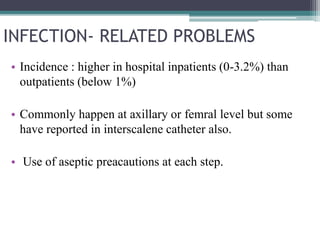
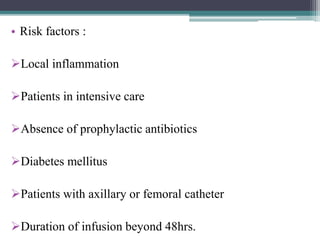
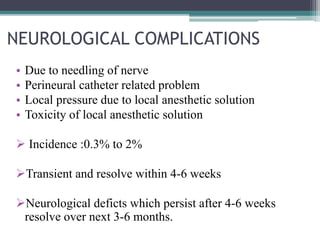
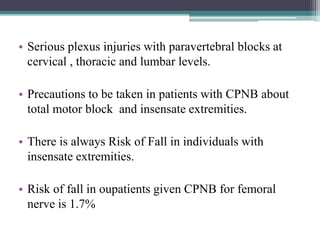
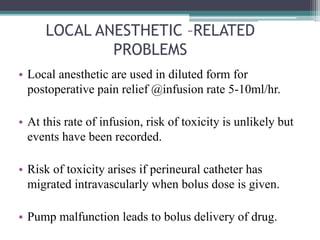
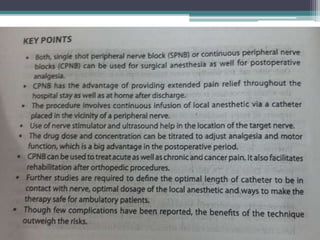
This document provides an overview of continuous peripheral nerve blocks (CPNBs). It discusses the preference for CPNBs over single-shot peripheral nerve blocks to provide continuous postoperative pain relief without breakthrough pain. It covers the history, indications, contraindications, techniques using nerve stimulators and ultrasound, common medications and delivery methods, anticoagulation considerations, potential complications, and key points about infection risks and neurological issues. The document aims to educate on the use of CPNBs for effective postoperative analgesia management in both inpatient and outpatient settings.