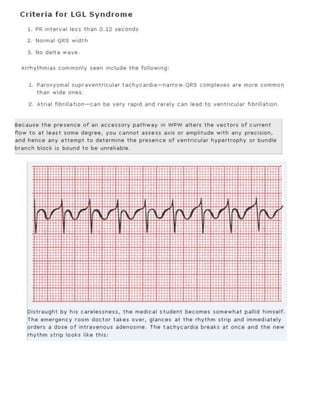
The 11-step method provides a systematic approach to reading EKGs:
1. Gather data such as heart rate, intervals, and axis.
2. Diagnose rhythm, conduction blocks, enlargement, and infarction by applying specific criteria.
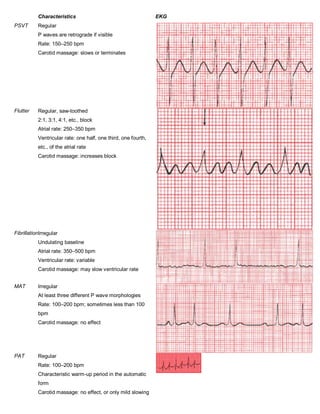
3. Potential diagnoses are identified through disturbances of rhythm, conduction, hypertrophy, and ischemia. The four questions framework is used to characterize rhythms.
![The 11-Step Method for Reading EKGs
Data Gathering
1. Standardization. Make sure the standardization mark on the EKG paper is 10 mm high so that 10 mm = 1 mV. Also make sure that
the paper speed is correct.
2. Heart rate. Determine the heart rate by the quick three-step method = [ 3 : large squares]
3. Intervals. Measure the length of the PR and QT intervals and the width of the QRS complexes.
4. QRS axis. Is the axis normal, or is there axis deviation?
Diagnoses
5. Rhythm. Always ask The Four Questions:
o Are there normal P waves present?
o Are the QRS complexes wide or narrow?
o What is the relationship between the P waves and QRS complexes?
o Is the rhythm regular or irregular?
6. AV block. Apply the criteria
7. Bundle branch block or hemiblock. Apply the criteria
8. Preexcitation. Apply the criteria
(Note that steps 6 through 8 all involve looking for disturbances of conduction.
9. Enlargement and hypertrophy. Apply the criteria for both atrial enlargement and ventricular hypertrophy.
10. Coronary artery disease. Look for Q waves and ST segment and T wave changes. Remember that not all such changes
reflect coronary artery disease; know your differential diagnoses.
11. Utter confusion. Is there anything on the EKG you don't understand? Never hesitate to ask for assistance.
information only becomes knowledge with wisdom and experience](https://image.slidesharecdn.com/44ecg-100105105558-phpapp01/75/44-E-C-G-1-2048.jpg)