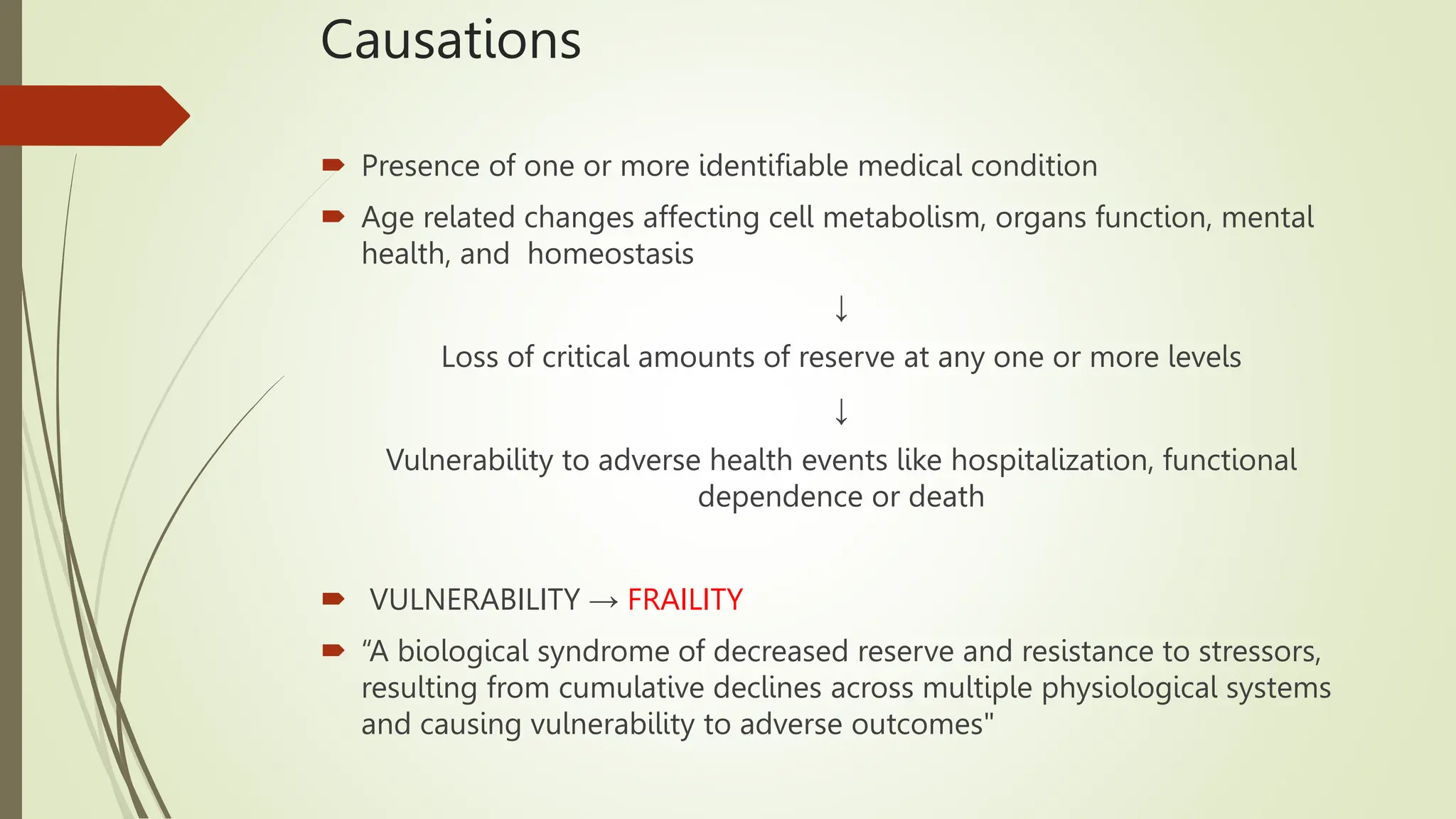
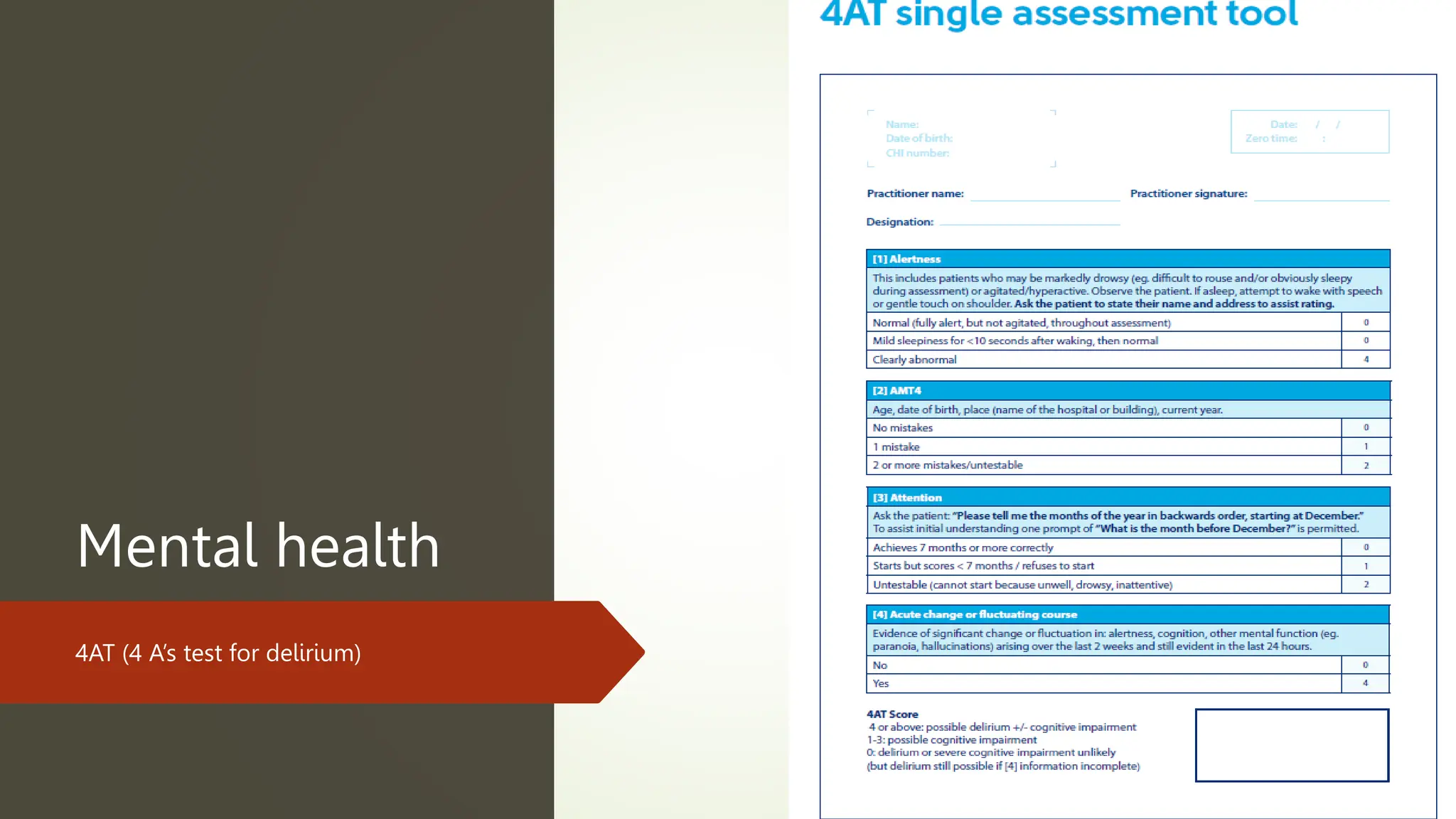
The document discusses the importance of comprehensive geriatric assessment (CGA) from a physiotherapy perspective, highlighting the increasing elderly population and the need for effective health care to address functional limitations and frailty. It outlines the assessment process, core principles, and the necessity of interdisciplinary approaches to develop holistic treatment plans. The document emphasizes functional assessments in older adults, particularly over 75, and details various assessment tools for evaluating mobility, balance, and other functional capabilities.