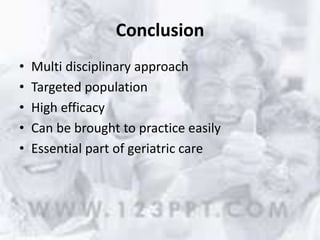
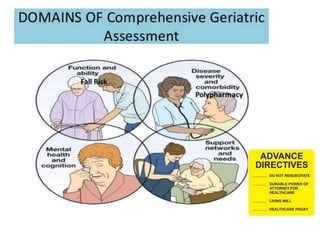
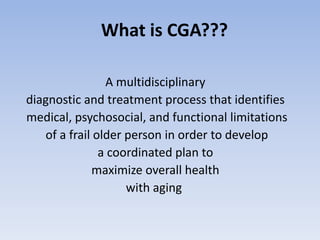
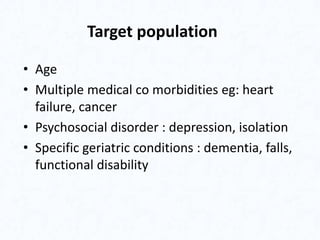
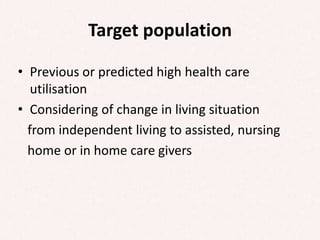
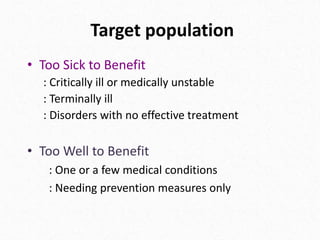
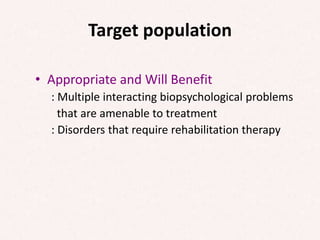
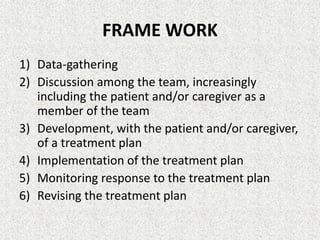
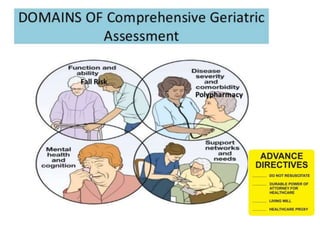
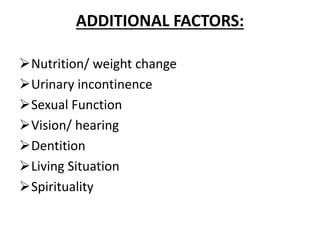
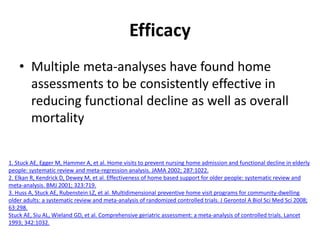
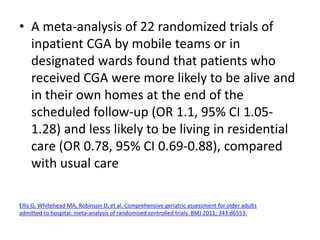
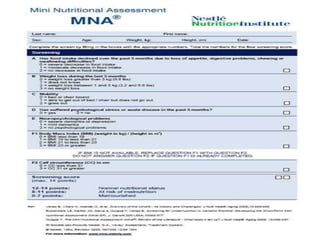
Comprehensive geriatric assessment (CGA) is a multidisciplinary process to assess medical, psychological, and functional limitations in frail older adults to develop a coordinated care plan. It involves a 3-step process of targeting appropriate patients, assessing patients across domains, and implementing recommendations from the multidisciplinary team. Meta-analyses have found CGA to be effective in reducing functional decline, mortality, and nursing home admissions. Key domains assessed include cognition, mood, functional status, nutrition, vision, hearing, continence, social support, medications, and advance care planning.



![• 17 randomized trials evaluating geriatric
rehabilitative units (within an acute care
hospital or a rehabilitation hospital) found that
inpatient multidisciplinary programs were
associated with improvement in all outcomes
at discharge, including better functional status
(OR 1.75, 95% CI 1.31-2.35), decreased nursing
home admission (relative risk [RR] 0.64, 0.51-
0.81), and reduced mortality (RR 0.72, 0.55-
0.95).
Bachmann S, Finger C, Huss A, et al. Inpatient rehabilitation specifically designed for geriatric patients:
systematic review and meta-analysis of randomised controlled trials. BMJ 2010; 340:c1718.](https://image.slidesharecdn.com/comprehensivegeriatricassessment-180327151502/85/Comprehensive-geriatric-assessment-16-320.jpg)






![NEWER APPLICATIONS OF CGA
• cancer patients undergoing chemotherapy [1]
• considerations of surgery, or transcatheter
aortic valve replacement for patients with
aortic stenosis [2]
• postoperative mortality risk [3].
1. Kalsi T, Babic-Illman G, Ross PJ, et al. The impact of comprehensive geriatric assessment interventions on tolerance to
chemotherapy in older people. Br J Cancer 2015; 112:1435.
2. Boureau AS, Trochu JN, Colliard C, et al. Determinants in treatment decision-making in older patients with symptomatic
severe aortic stenosis. Maturitas 2015; 82:128.
3. Kim SW, Han HS, Jung HW, et al. Multidimensional frailty score for the prediction of postoperative mortality risk. JAMA
Surg 2014; 149:633.](https://image.slidesharecdn.com/comprehensivegeriatricassessment-180327151502/85/Comprehensive-geriatric-assessment-45-320.jpg)