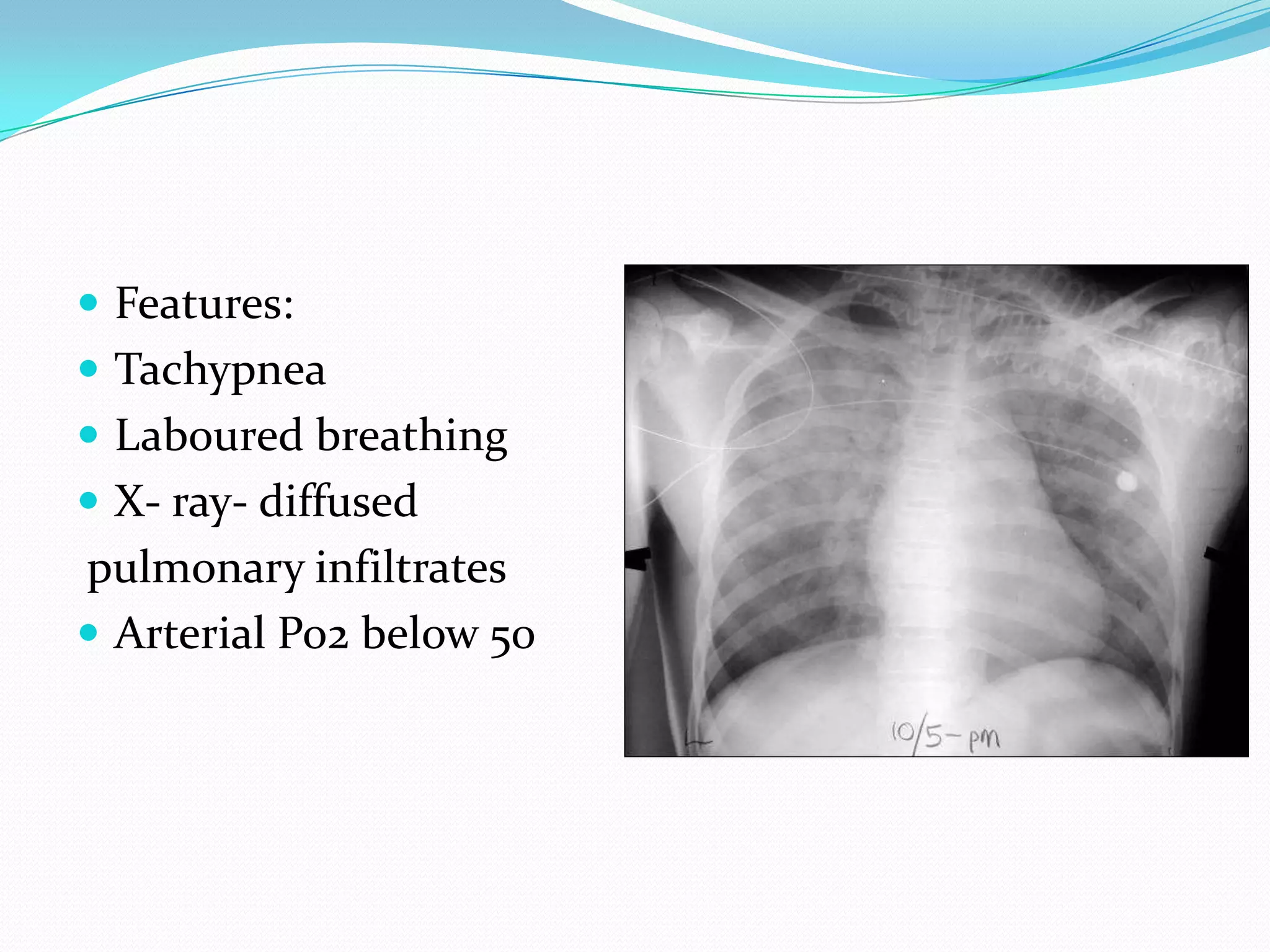
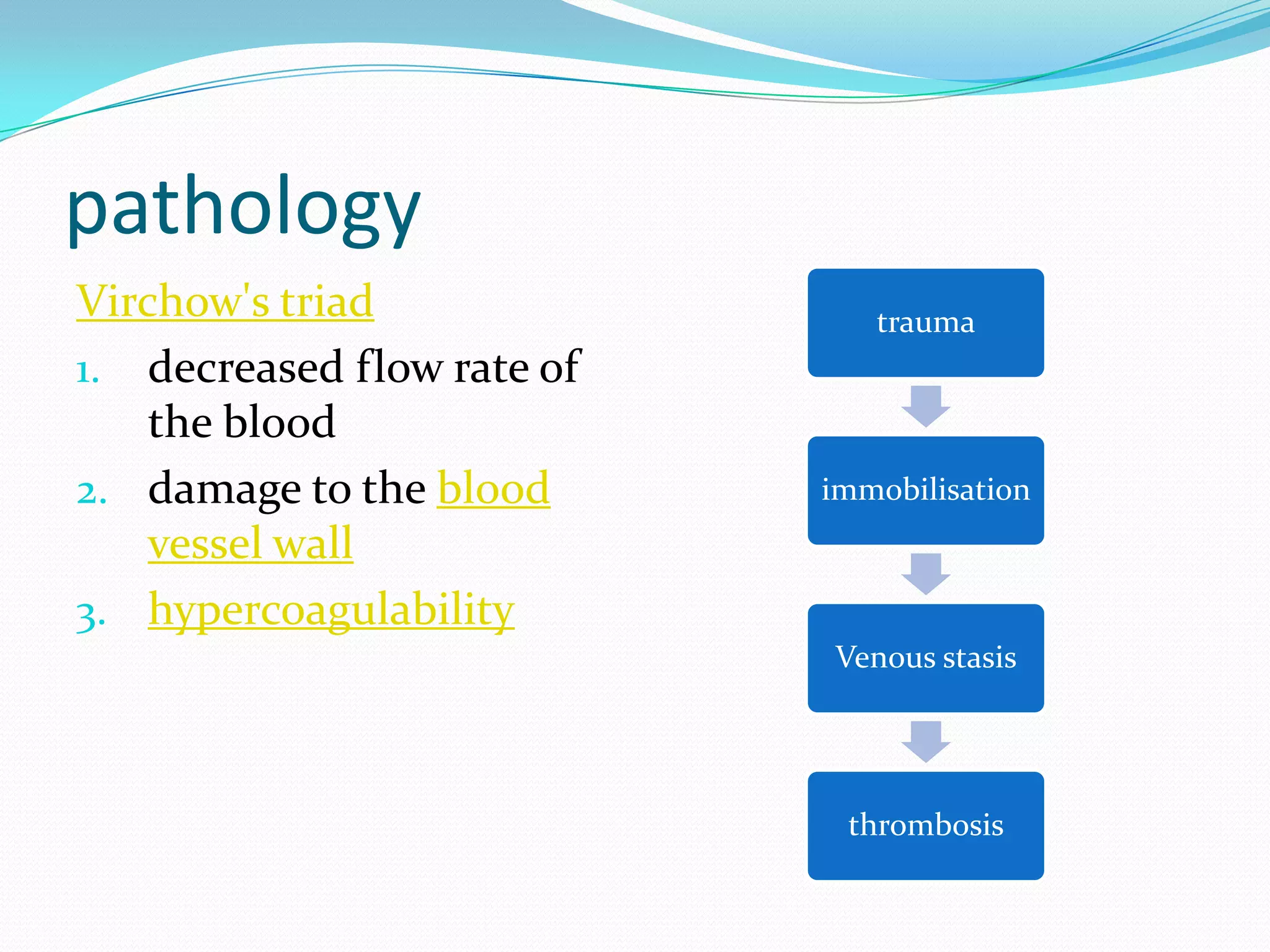
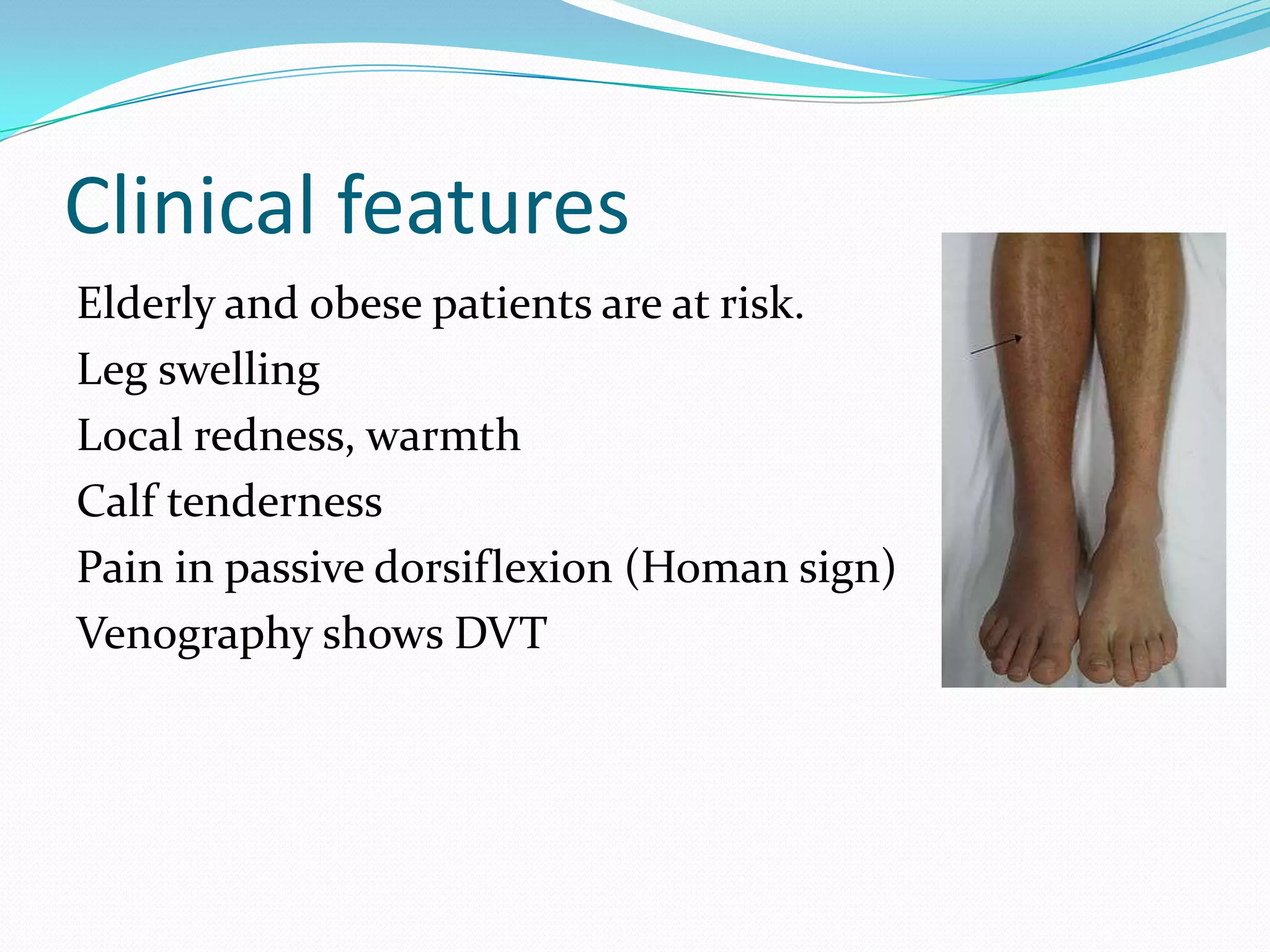
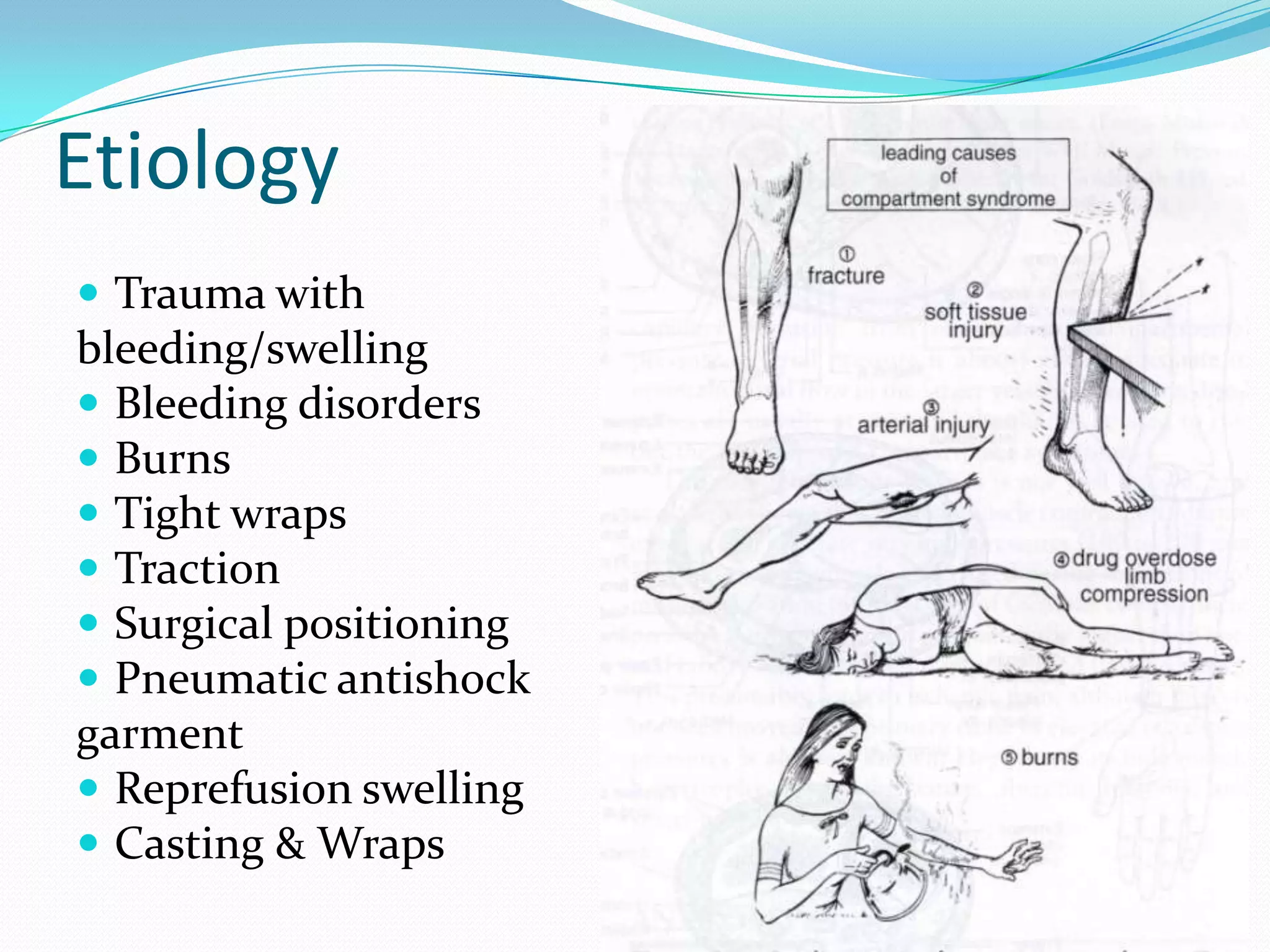
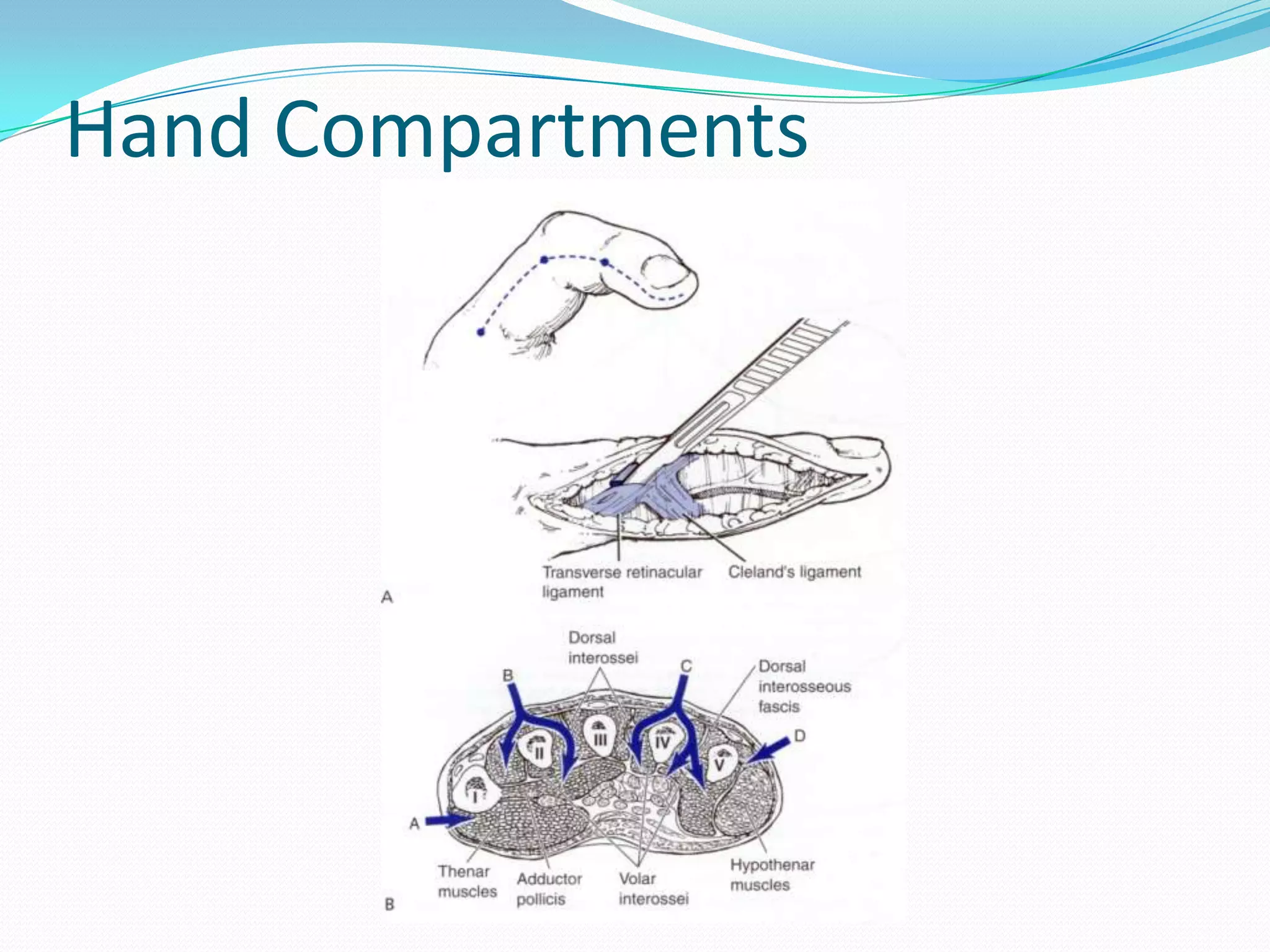
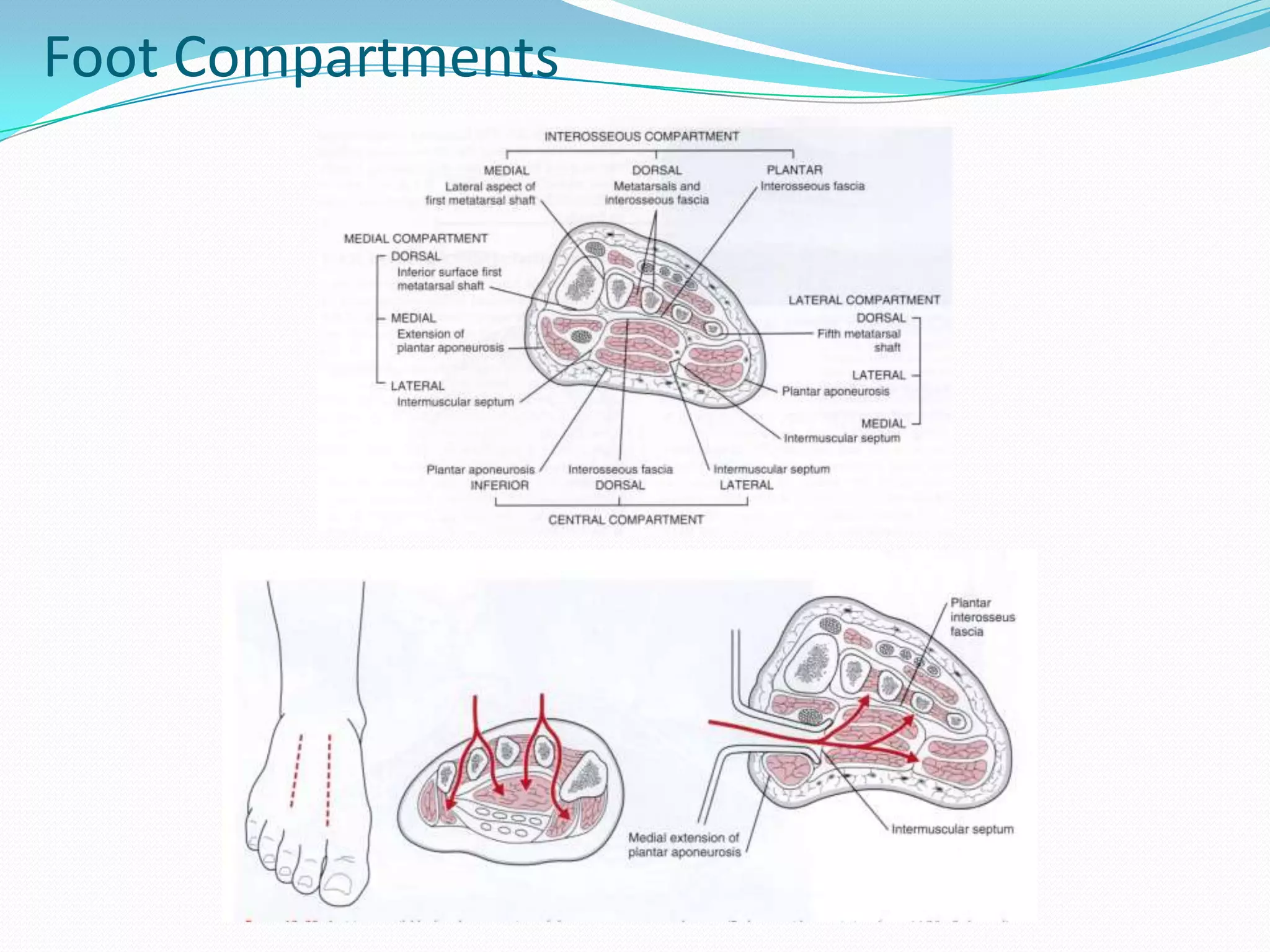
This document discusses various complications that can arise from fractures. It classifies complications as immediate, early, or late. Immediate complications include hypovolaemic shock, injuries to major vessels or internal organs. Early complications include hypovolaemic shock, ARDS, fat embolism, DVT, and infections. Late complications are related to imperfect union like delayed union, non-union, or malunion. Other late complications include avascular necrosis, joint stiffness, osteomyelitis, and osteoarthritis. The document provides details on pathogenesis, clinical features, diagnosis, and management of various common complications like hypovolaemic shock, fat embolism, DVT, crush syndrome, compartment syndrome, and