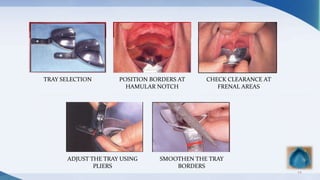
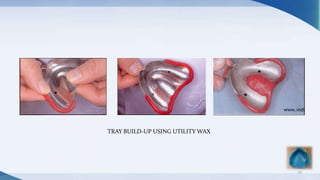
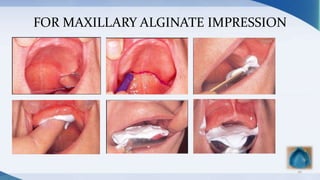
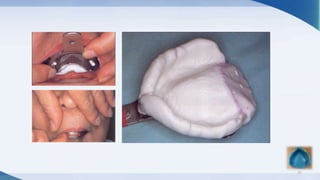
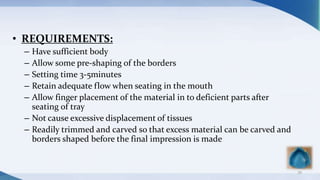
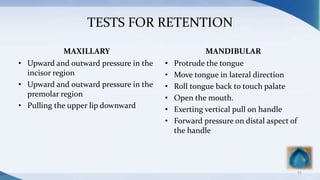
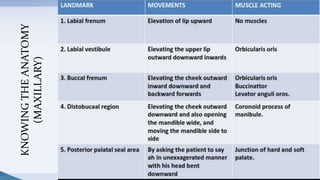
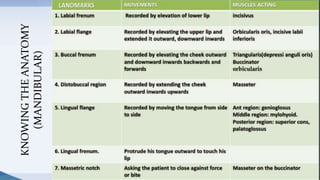
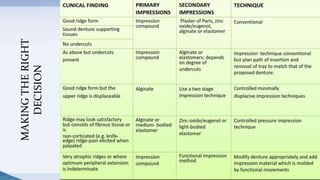
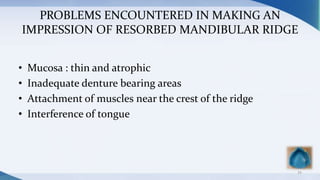
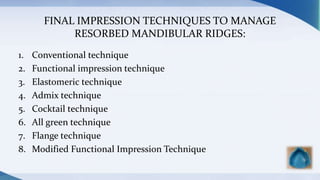
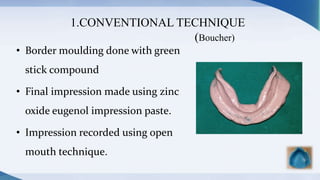
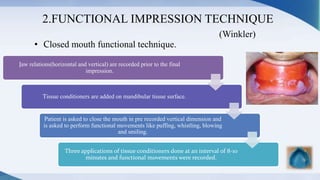
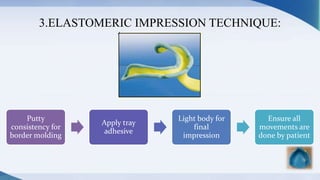
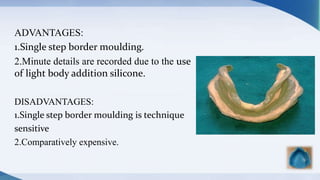
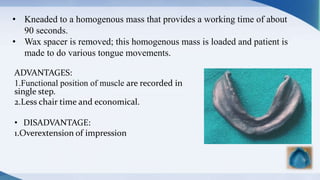
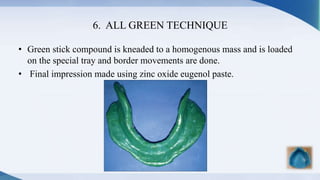
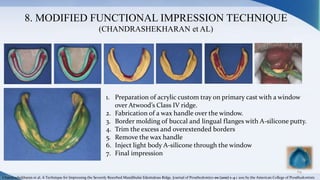
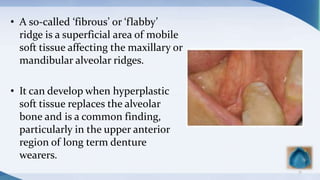
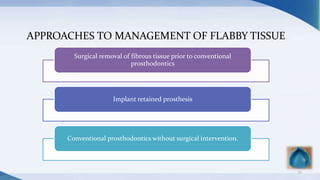
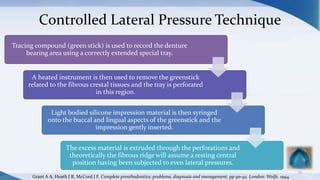
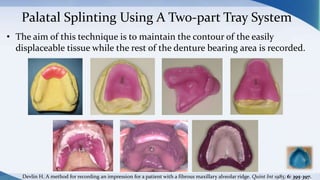
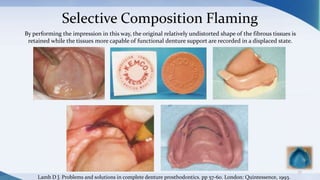
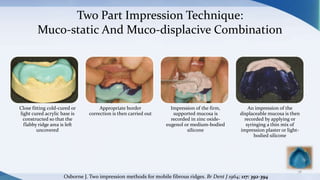
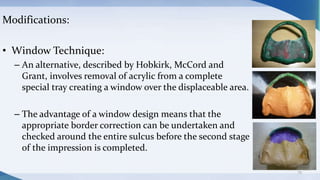
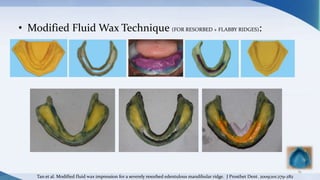
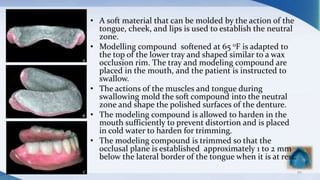
This document discusses various techniques for making impressions for complete dentures. It covers topics like border molding, anatomical considerations for different ridge types, and specialized techniques for resorbed or flabby ridges. For resorbed mandibular ridges, techniques discussed include the conventional, functional, elastomeric, admix, cocktail, and modified functional impression techniques. For flabby ridges, the mucodisplacive and mucostatic impression principles are covered, as well as the one part impression and controlled lateral pressure techniques. The document provides details on selecting the appropriate impression material and technique based on a patient's clinical situation.