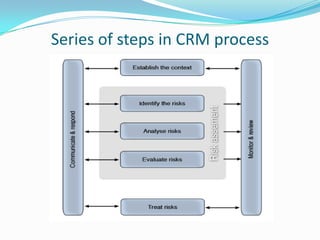
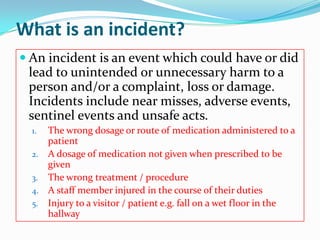
1) Clinical risk management (CRM) aims to improve healthcare quality and safety by identifying and preventing circumstances that put patients at risk of harm.
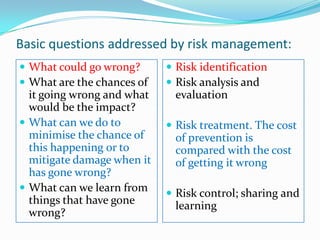
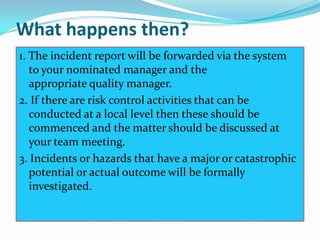
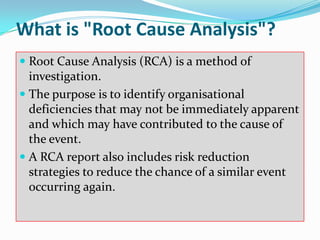
2) Risk management involves risk identification, analysis, treatment, and control to minimize chances of errors and learn from past issues.
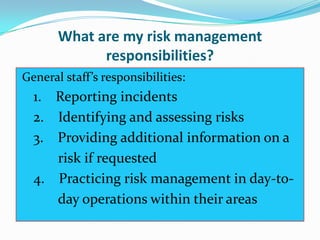
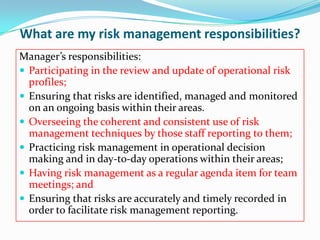
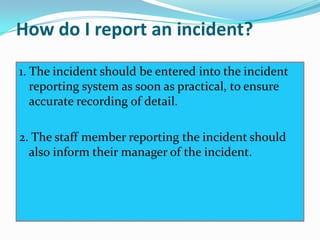
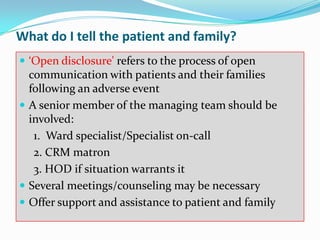
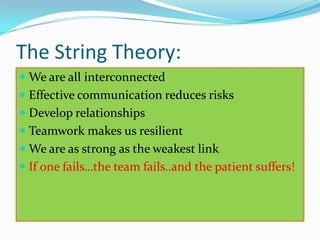
3) All healthcare staff have responsibilities for risk management including reporting incidents, identifying risks, and practicing risk prevention in their daily work.