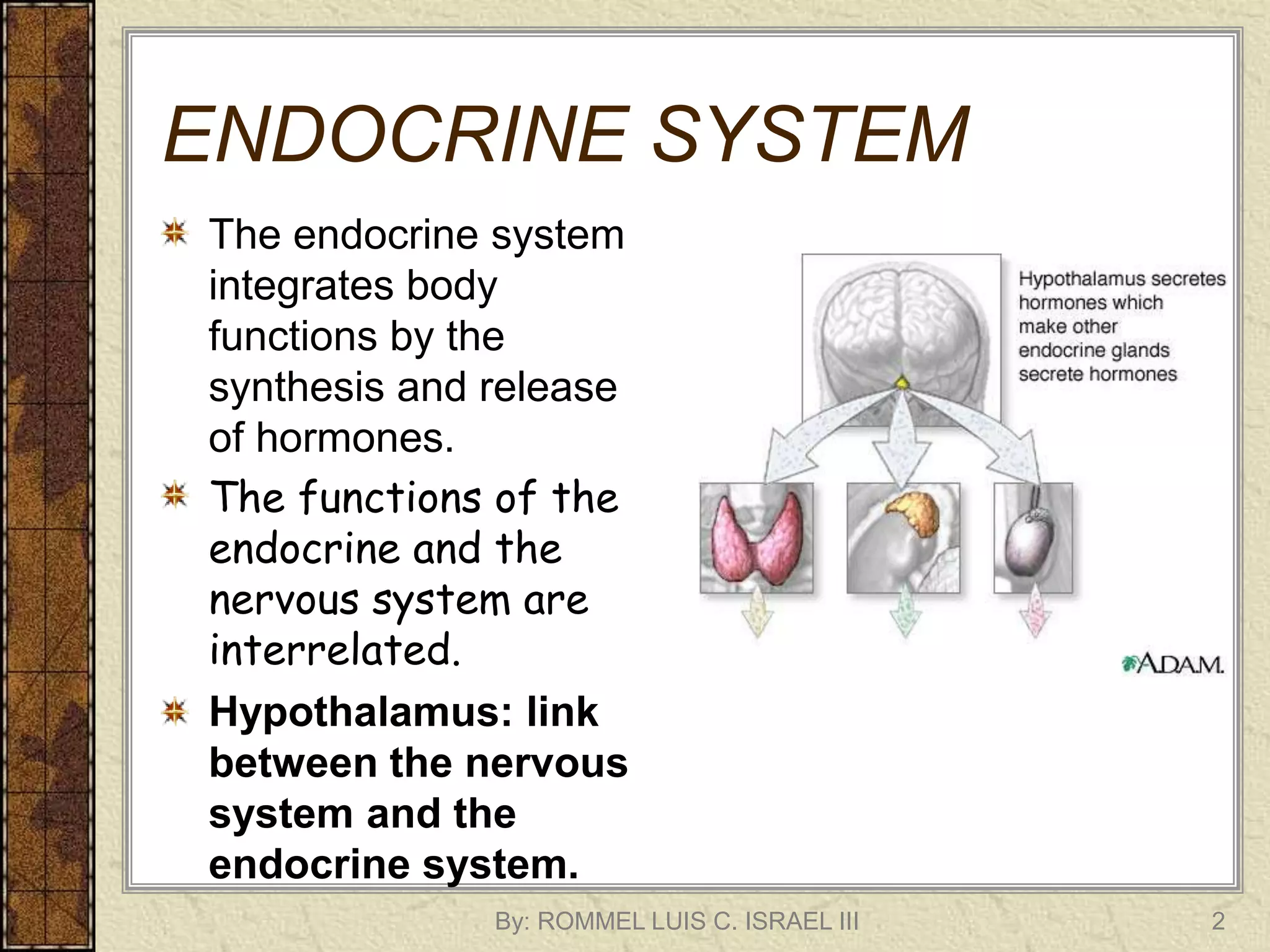
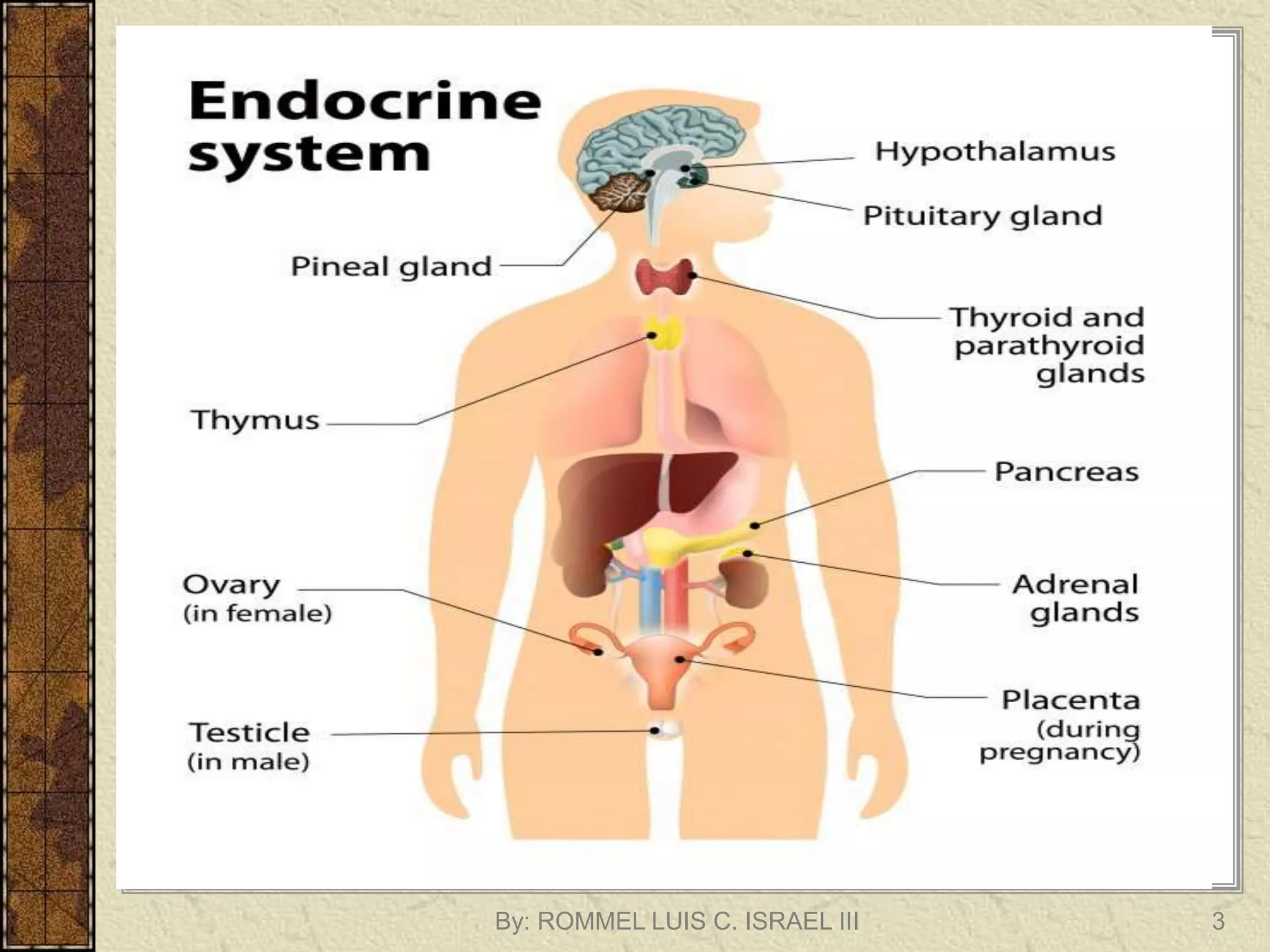
The endocrine system regulates body functions through the synthesis and release of hormones from endocrine glands. The hypothalamus links the nervous and endocrine systems by stimulating or inhibiting hormone release from the pituitary gland. The pituitary gland, known as the "master gland", regulates other endocrine glands and organs by producing hormones that signal the release of other hormones. Key endocrine glands include the thyroid, adrenals, pancreas, ovaries/testes, and parathyroids, each producing hormones that regulate processes like metabolism, stress response, growth, and reproduction.

































































































































































































































































![References:
Oxytocin | You and Your Hormones from the Society for Endocrinology. (n.d.).
Www.yourhormones.info.
https://www.yourhormones.info/hormones/oxytocin/#:~:text=by%20the%20nipple.-
US EPA, O. (2015, July 6). Overview of the Endocrine System. Www.epa.gov.
https://www.epa.gov/endocrine-disruption/overview-endocrine-
system#:~:text=The%20endocrine%20system%2C%20made%20up
Hypothalamus: Function, hormones, and disorders. (n.d.). Www.medicalnewstoday.com.
https://www.medicalnewstoday.com/articles/312628#disorders
Biology LibreTexts. (2016). 13.27: Hormone Regulation. [online] Available at:
https://bio.libretexts.org/Bookshelves/Introductory_and_General_Biology/Introductory_Biology_(
CK-
12)/13%3A_Human_Biology/13.27%3A_Hormone_Regulation#:~:text=Most%20hormones%20are
%20controlled%20by.
Better Health (2017). Growth hormone. [online] Vic.gov.au. Available at:
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/growth-hormone.
Allen, M.J. and Sharma, S. (2021). Physiology, Adrenocorticotropic Hormone (ACTH). [online] PubMed. Available at:
https://www.ncbi.nlm.nih.gov/books/NBK500031/#:~:text=Adrenocorticotropic%20hormone%20(ACTH)%20is%20a.
By: ROMMEL LUIS C. ISRAEL III 263](https://image.slidesharecdn.com/endocrinesystemlecture-230902084004-27cf0b64/75/CLIENTS-WITH-PROBLEMS-IN-ENDOCRINE-SYSTEM-261-2048.jpg)
![References:
Shomon, M. (2004). High and Low TSH Levels: What They Mean. [online] Verywell Health. Available
at: https://www.verywellhealth.com/understanding-thyroid-blood-tests-low-or-high-tsh-3233198.
Luteinizing and Follicle Stimulating Hormones. (n.d.). Www.vivo.colostate.edu.
http://www.vivo.colostate.edu/hbooks/pathphys/endocrine/hypopit/lhfsh.html#:~:text=Luteinizin
g%20hormone%20%28LH%29%20and%20follicle-stimulating%20hormone%20%28FSH%29%20are
Yourhormones.info. (2018). Melanocyte-stimulating hormone | You and Your Hormones from the
Society for Endocrinology. [online] Available at:
https://www.yourhormones.info/hormones/melanocyte-stimulating-hormone/.
Melanocyte-stimulating hormone | You and Your Hormones from the Society for Endocrinology.
(2018). Yourhormones.info. https://www.yourhormones.info/hormones/melanocyte-stimulating-
hormone/
Verywell Health. (n.d.). A Quick Rundown of the Symptoms of Hypogonadism. [online] Available at:
https://www.verywellhealth.com/hypogonadism-signs-symptoms-and-complications-5191935.
Bing. (n.d.). Transsphenoidal hypophysectomy. [online] Available at:
https://www.bing.com/search?q=Transsphenoidal+hypophysectomy&cvid=349c865c86eb4249a78
60659ce931476&aqs=edge..69i57j0l8.1337j0j4&FORM=ANAB01&PC=NMTS [Accessed 13 Aug.
2023].
By: ROMMEL LUIS C. ISRAEL III 264](https://image.slidesharecdn.com/endocrinesystemlecture-230902084004-27cf0b64/75/CLIENTS-WITH-PROBLEMS-IN-ENDOCRINE-SYSTEM-262-2048.jpg)
![References:
• Mayo Clinic (2021). Diabetes insipidus - Symptoms and causes. [online] Mayo
Clinic. Available at: https://www.mayoclinic.org/diseases-conditions/diabetes-
insipidus/symptoms-causes/syc-20351269.
• Vallie, S. (n.d.). What Is SIADH? [online] WebMD. Available at:
https://www.webmd.com/a-to-z-guides/what-is-siadh.
• Society for Endocrinology (2019). Adrenocorticotropic hormone | You and
Your Hormones from the Society for Endocrinology. [online]
Yourhormones.info. Available at:
https://www.yourhormones.info/hormones/adrenocorticotropic-hormone/.
• Australia, H. (2020). The role of cortisol in the body. [online]
www.healthdirect.gov.au. Available at: https://www.healthdirect.gov.au/the-
role-of-cortisol-in-the-
body#:~:text=Cortisol%20is%20a%20hormone%20produced.
By: ROMMEL LUIS C. ISRAEL III 265](https://image.slidesharecdn.com/endocrinesystemlecture-230902084004-27cf0b64/75/CLIENTS-WITH-PROBLEMS-IN-ENDOCRINE-SYSTEM-263-2048.jpg)