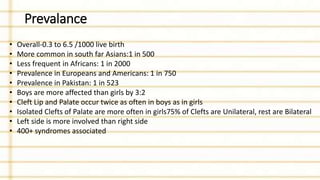
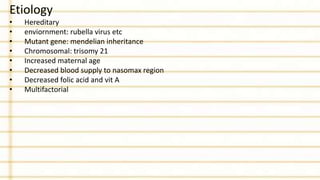
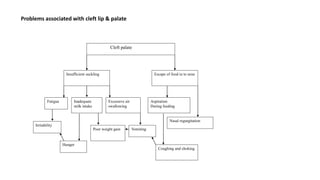
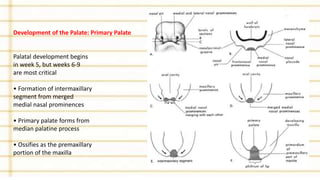
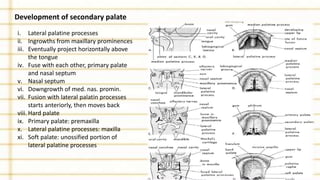
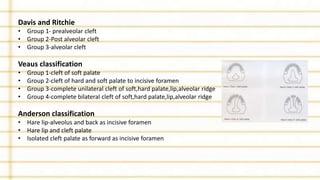
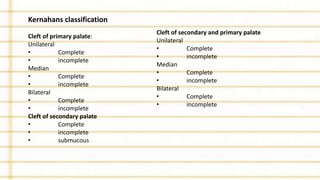
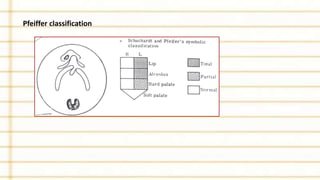
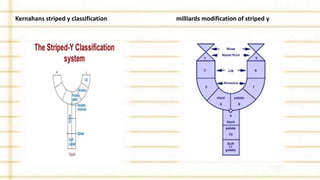
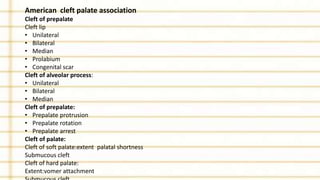
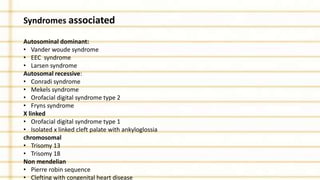
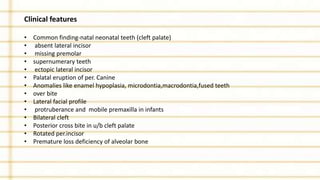
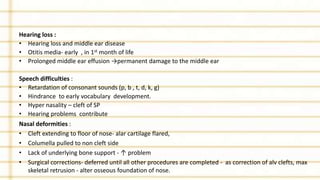
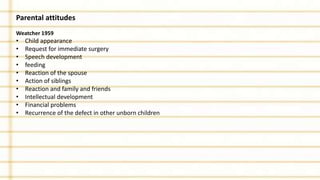
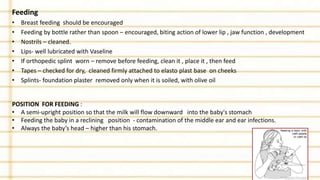
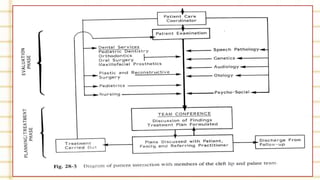
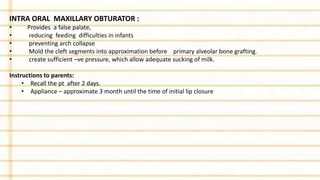
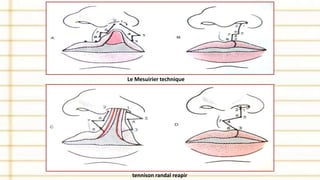
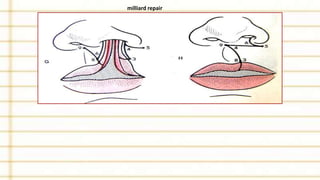
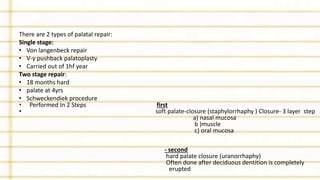
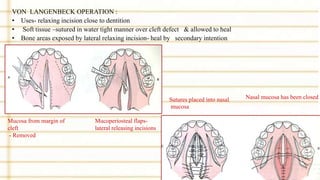
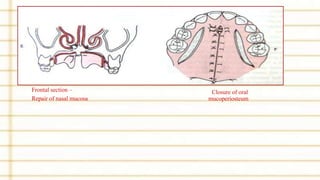
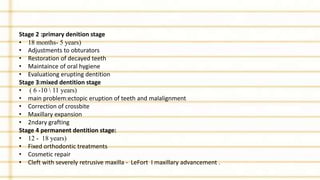
Management of cleft lip and palate involves a multidisciplinary team approach. The document discusses the history, classification, prevalence, etiology and development of clefts. It also covers clinical features, parental attitudes, feeding techniques, and the treatment plan which involves multiple stages including maxillary orthopedics, presurgical orthodontics, surgical lip and palate closure, and primary repair between 10-18 months of age. The goal is to surgically correct the deformity while addressing issues such as feeding, speech, and dental development.