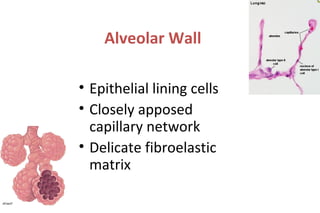
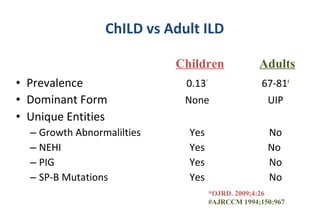
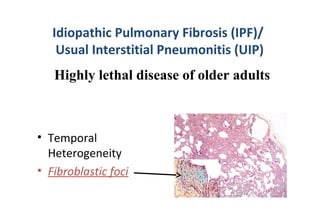
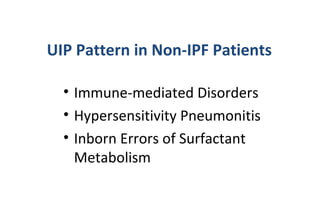
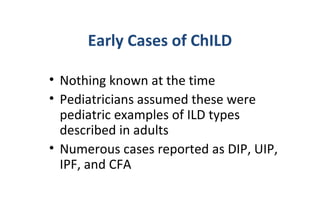
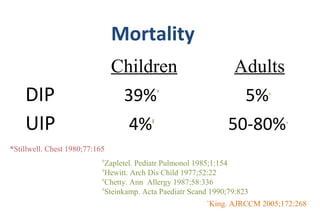
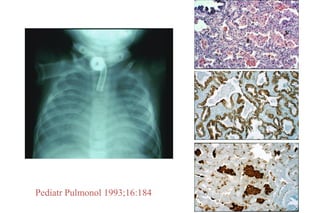
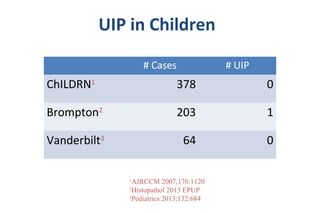
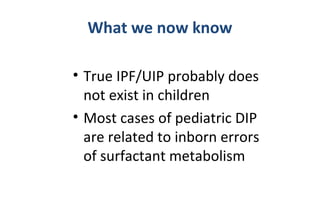
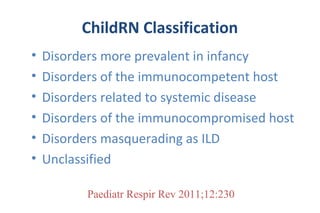
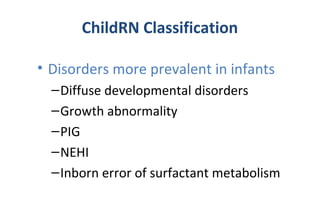
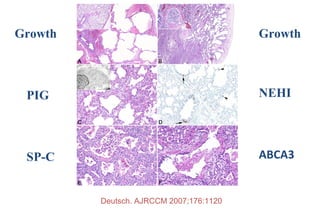
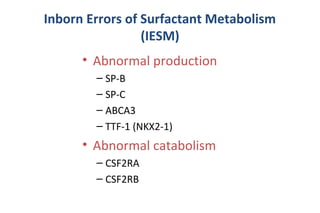
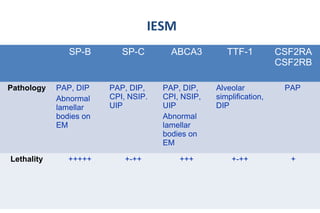
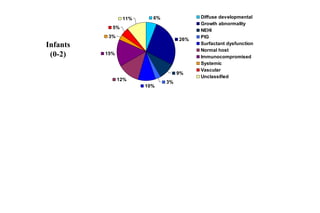
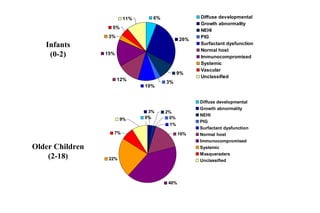
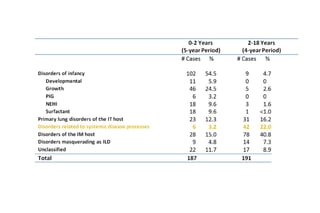
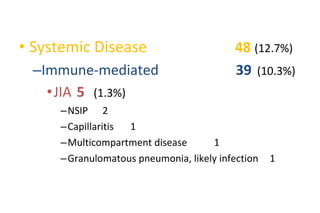
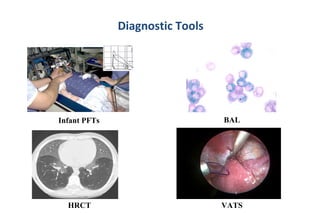
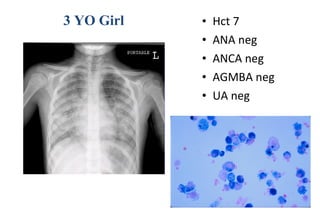
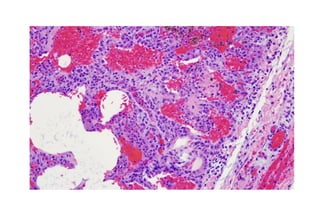
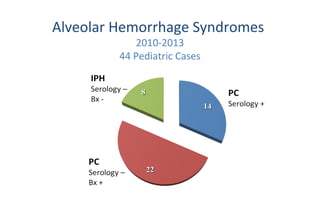
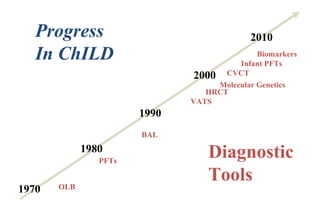
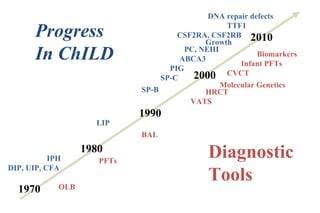
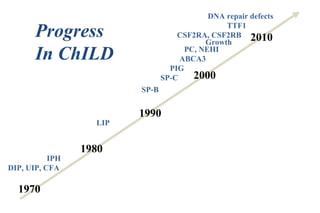
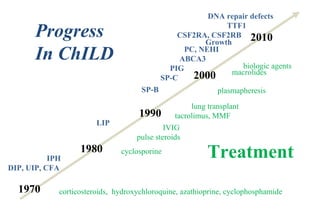
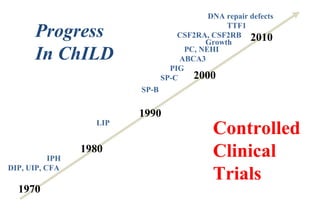
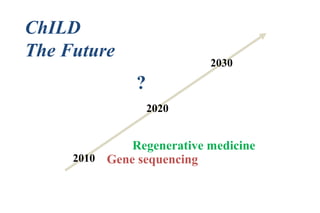
This document provides an overview of Children's Interstitial Lung Disease (ChILD). It discusses that ChILD is a heterogeneous group of rare lung disorders that cause damage to the alveolar walls. The prevalence and specific entities of ChILD differ from adult interstitial lung disease. ChILD can be difficult to diagnose due to its diversity and is associated with significant morbidity and mortality. Over time, diagnostic tools and understanding of ChILD have improved, leading to identification of genetic causes and targeted treatments. However, more research is still needed.