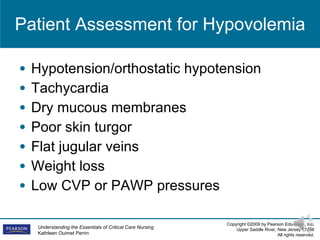
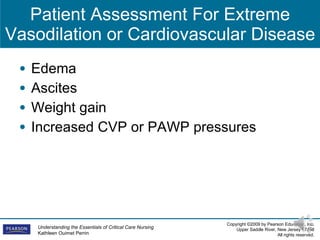
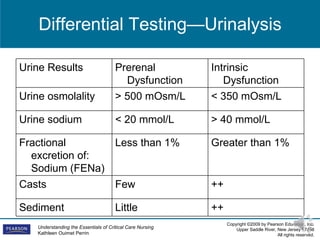
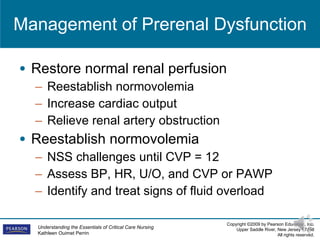
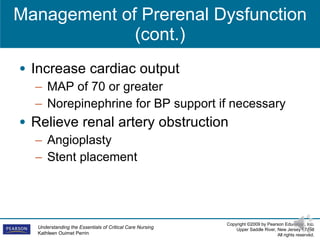
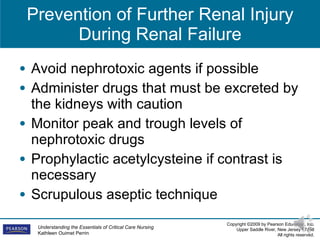
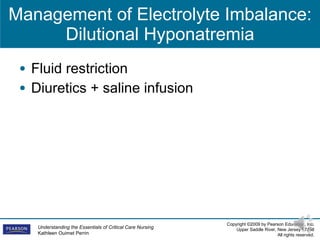
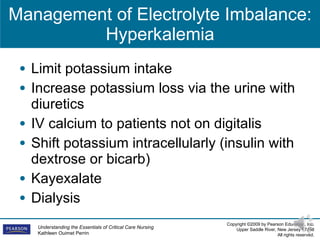
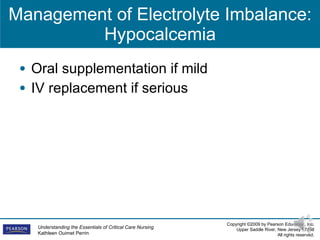
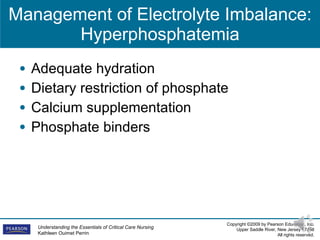
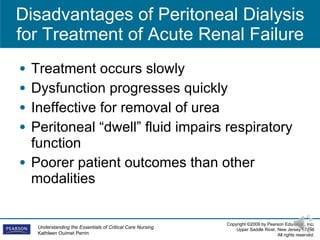
This document provides information on acute renal failure (ARF) including the causes, types, assessment, differential testing, management, and nursing care of patients with ARF requiring dialysis. It discusses the three main types of ARF - prerenal, intrarenal, and postrenal - and covers topics like fluid management, electrolyte imbalances, and the advantages and disadvantages of different renal replacement therapies including peritoneal dialysis, continuous renal replacement therapies, and hemodialysis.