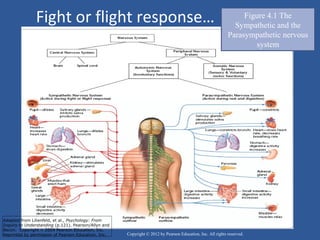
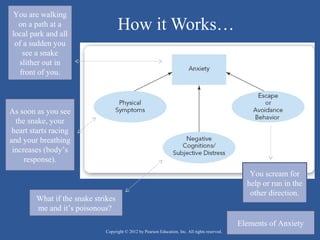
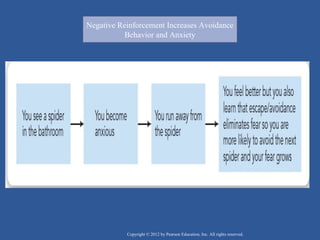
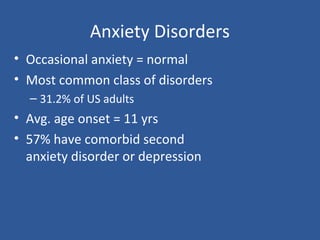
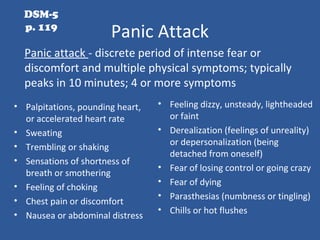
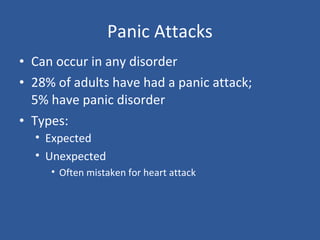
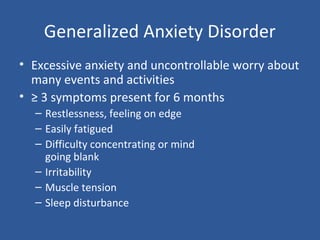
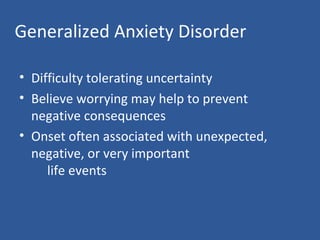
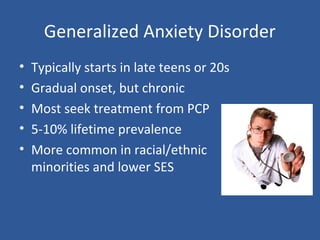
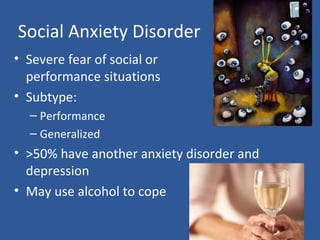
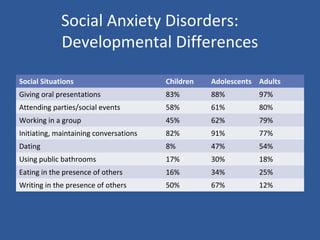
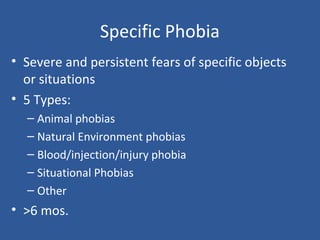
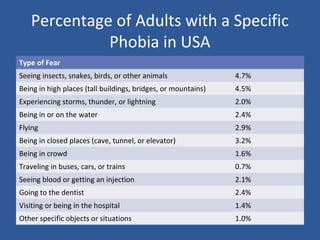
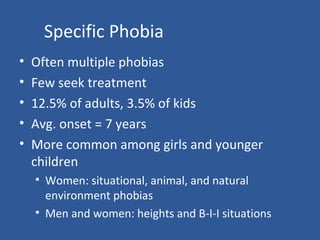
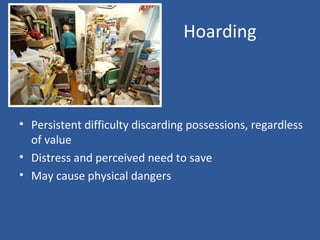
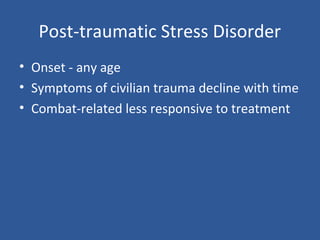
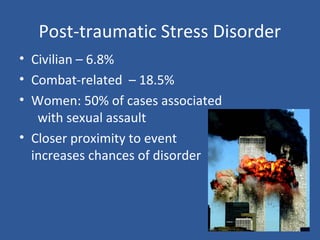
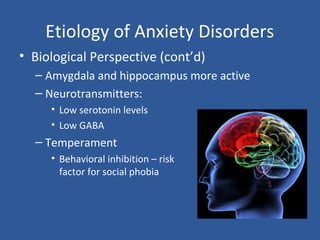
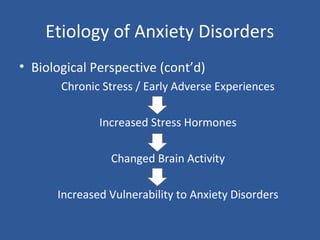
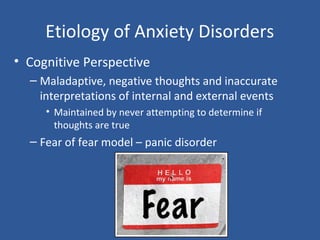
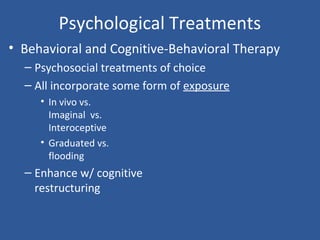
This document discusses the nature and types of anxiety disorders. It defines fear and anxiety, and describes the fight or flight response. The main types of anxiety disorders covered include generalized anxiety disorder, panic disorder, social anxiety disorder, specific phobias, obsessive-compulsive disorder, post-traumatic stress disorder, and their key symptoms. Biological, psychological, and cognitive factors that may contribute to the development and maintenance of anxiety disorders are also summarized.