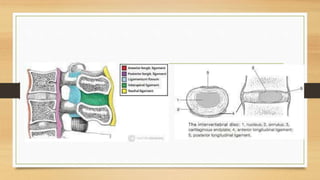
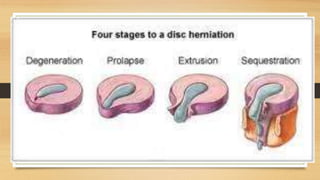
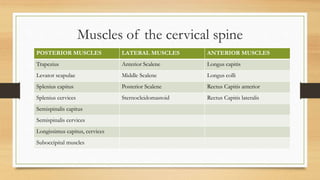
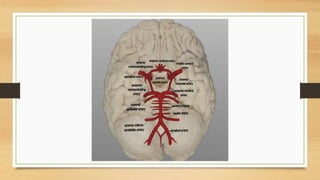
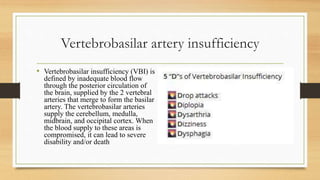
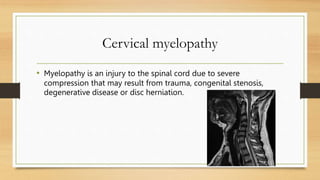
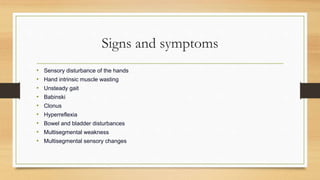
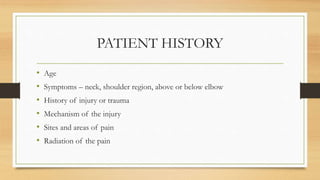
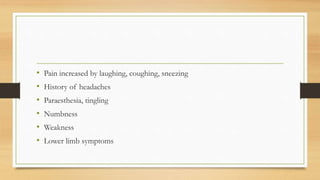
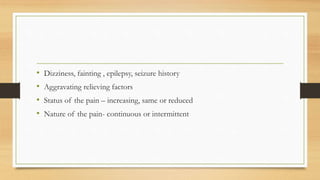
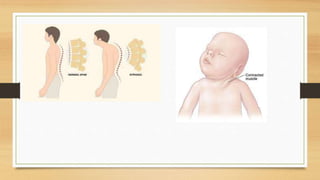
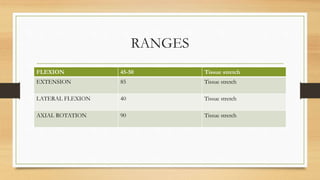
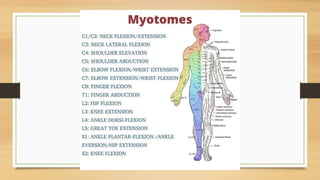
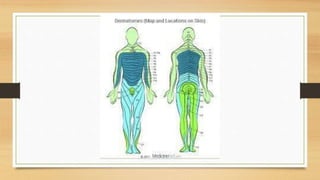
This document discusses the assessment of the cervical spine. It outlines the muscles of the cervical spine including posterior, lateral, and anterior muscles. It describes common signs and symptoms of cervical spine issues like pain, stiffness, numbness, and headaches. Red flags indicating more serious pathology are mentioned. The assessment involves taking a patient history, performing an examination of ranges of motion, reflexes, dermatomes, and special tests. Differential diagnoses that may be considered are also listed.