This document provides guidelines for cervical cancer screening including:
- Screening should start at age 21 and occur every 3 years until age 30, then every 3 years or every 5 years with HPV co-testing until age 65.
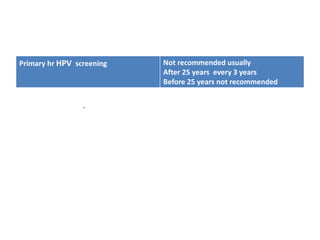
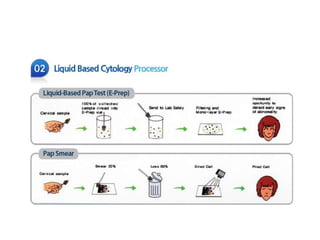
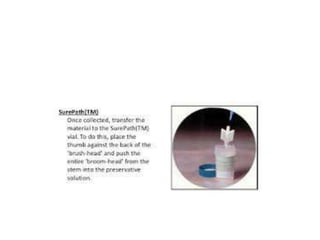
- Screening methods include cytology alone or HPV co-testing. Primary HPV testing is not usually recommended.
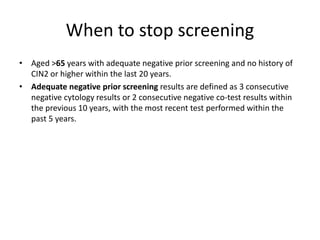
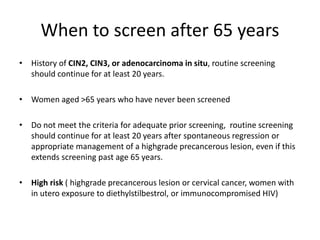
- Screening can stop after age 65 for those with adequate negative prior screening and no history of precancerous lesions in the past 20 years.