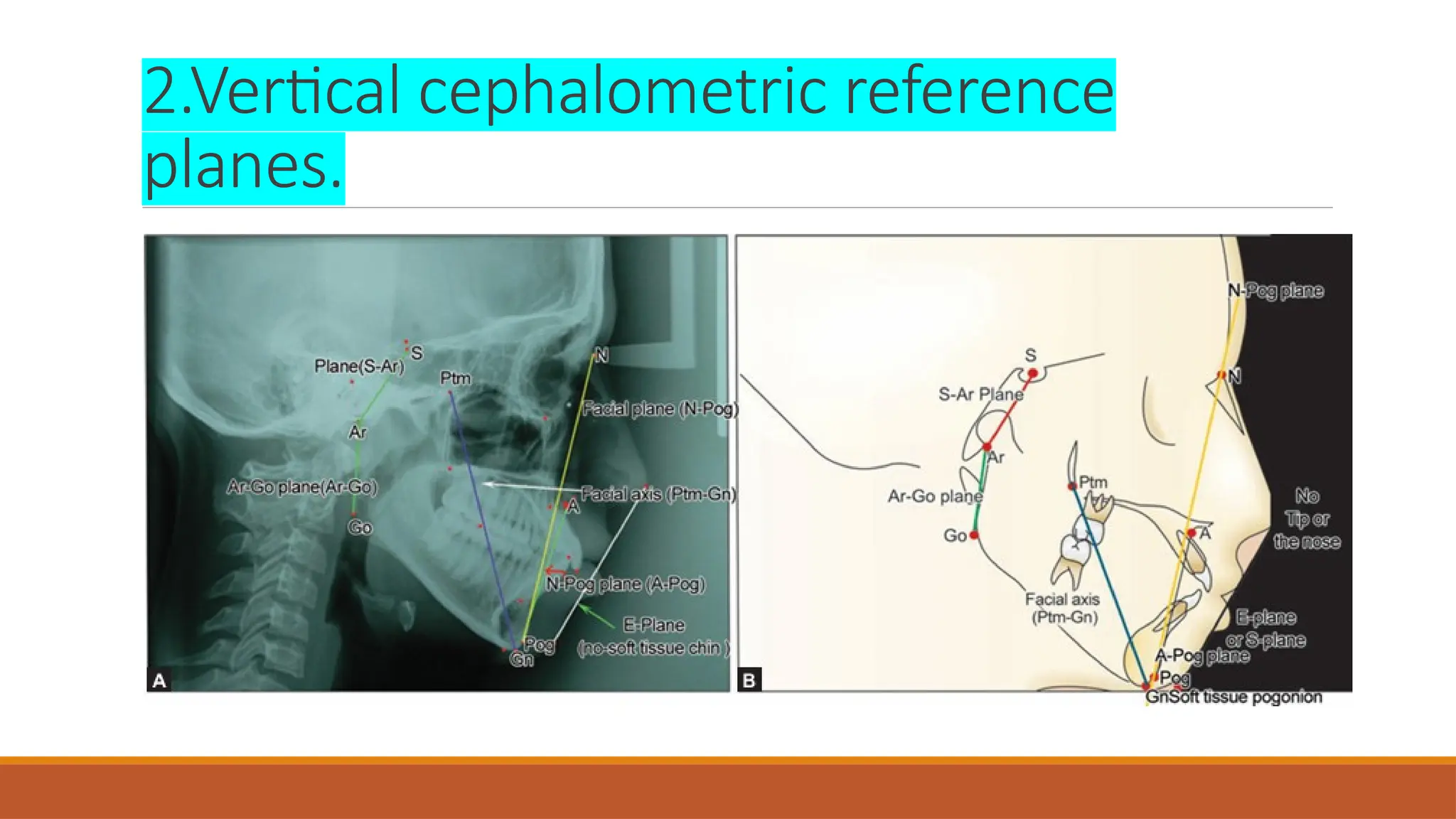
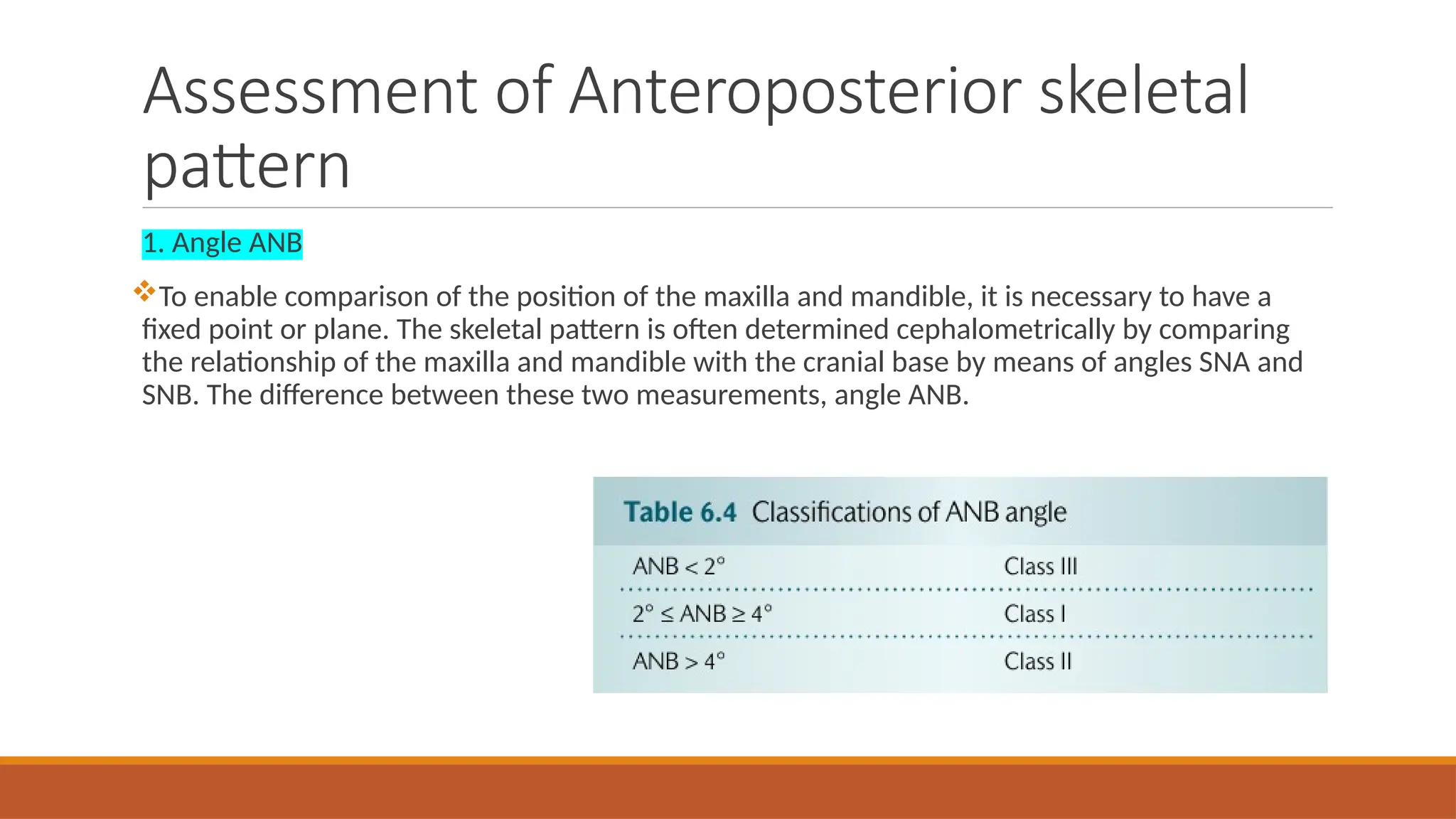
Cephalometric radiographs are essential in orthodontics for diagnosing and evaluating dental and facial relationships, monitoring treatment progress, and assessing treatment outcomes. They involve capturing standardized lateral and frontal images of the skull, which help in analyzing tooth movements and facial growth. Various landmarks and reference planes are used for accurate assessments, with both hand tracing and digitization methods available for further analysis.