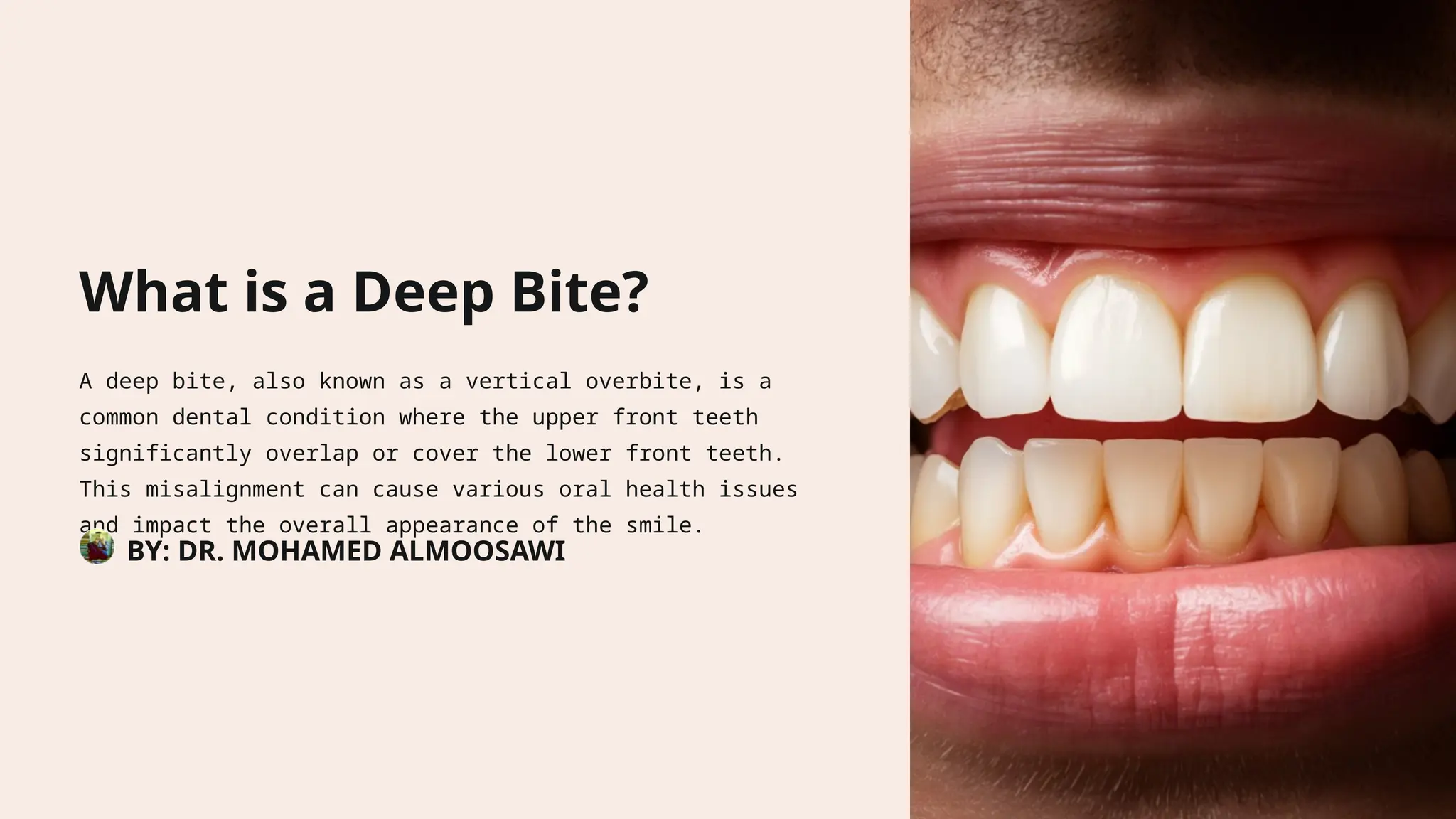
A deep bite, or vertical overbite, is a dental condition where the upper front teeth significantly overlap the lower front teeth, potentially causing oral health problems and affecting appearance. Factors such as genetics, tooth eruption patterns, muscle imbalances, and oral habits contribute to its development. Treatment may involve orthodontic interventions, growth modification, and, in severe cases, surgical correction to restore proper function and aesthetics.