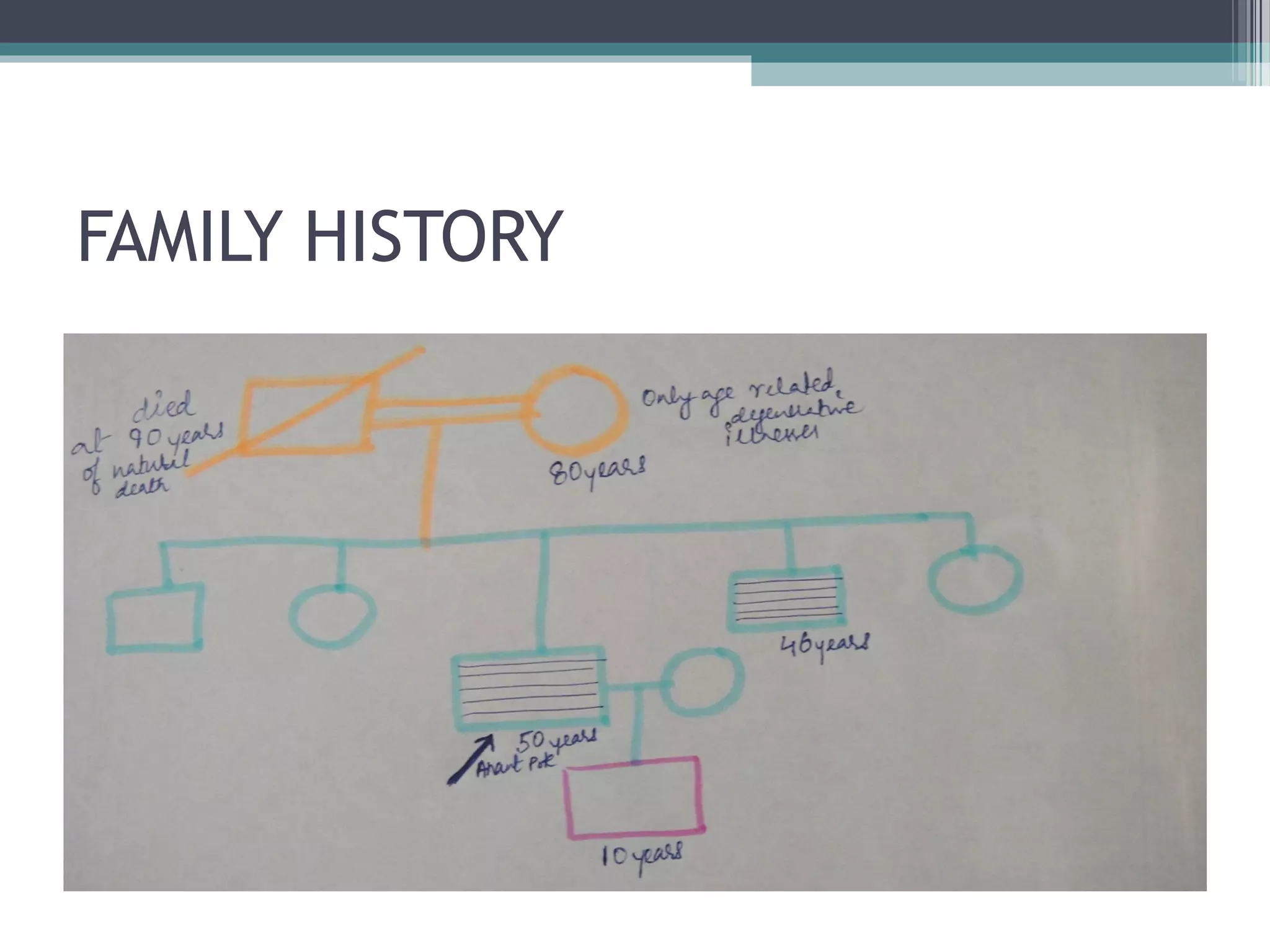
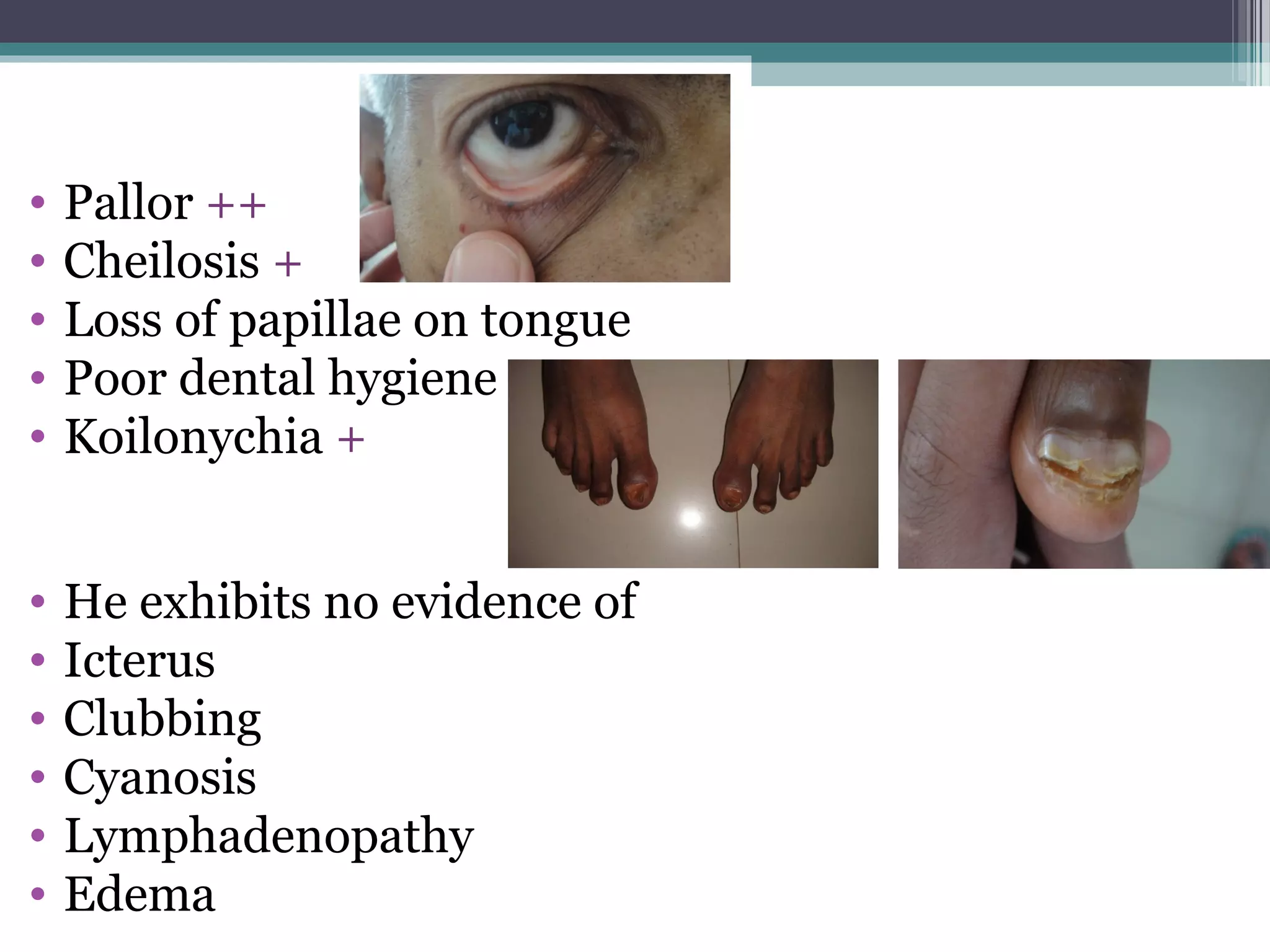
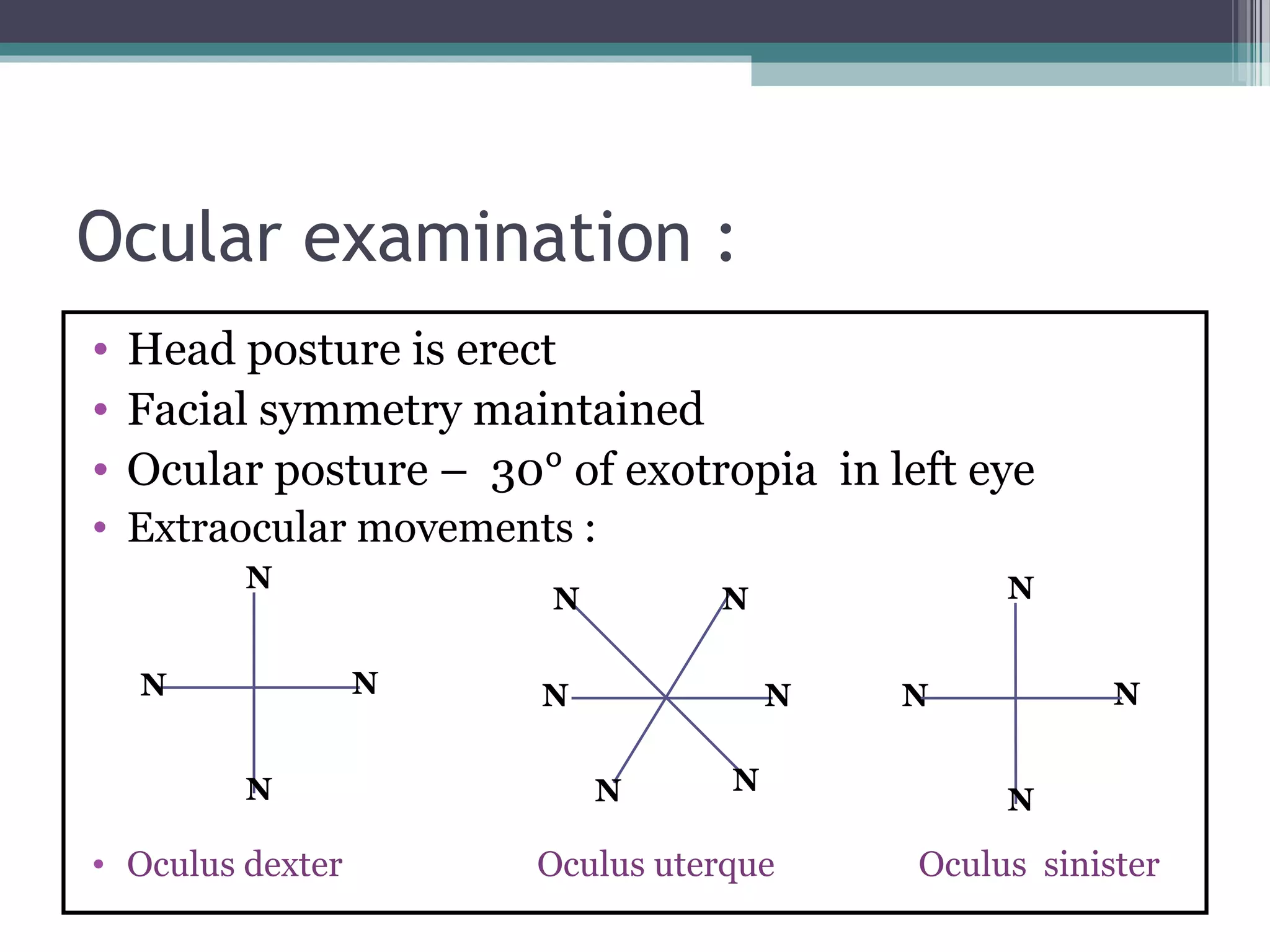
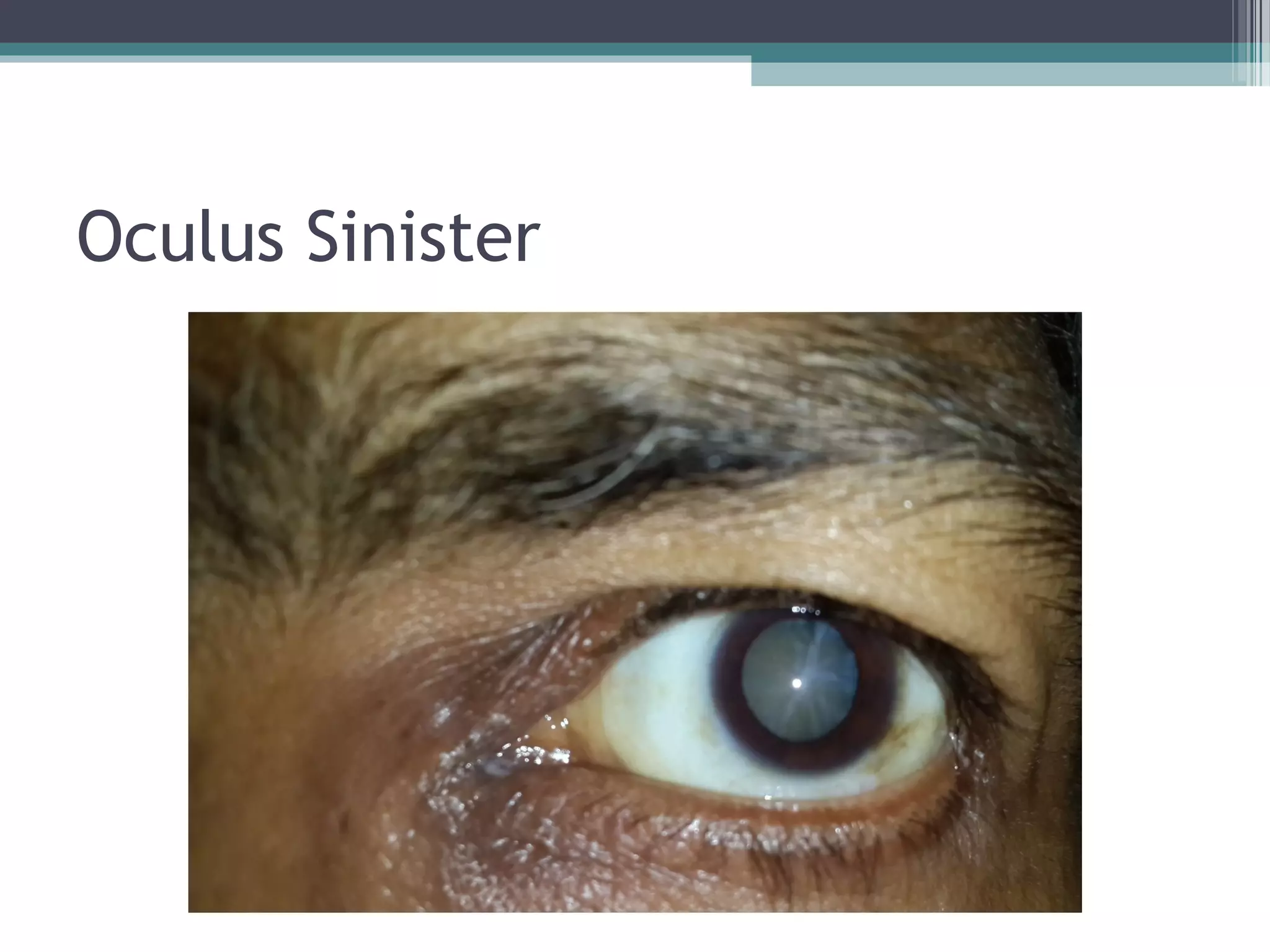
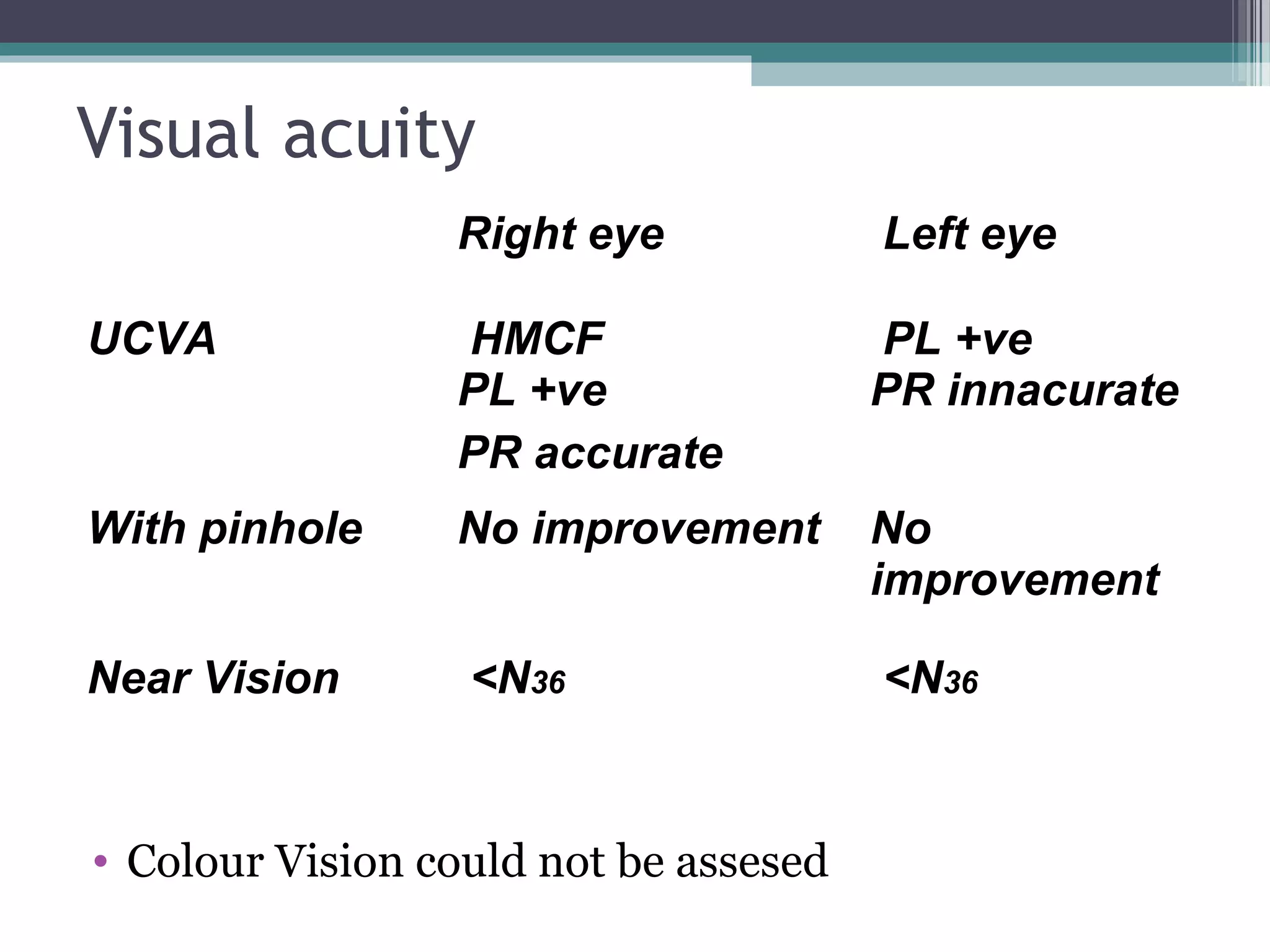
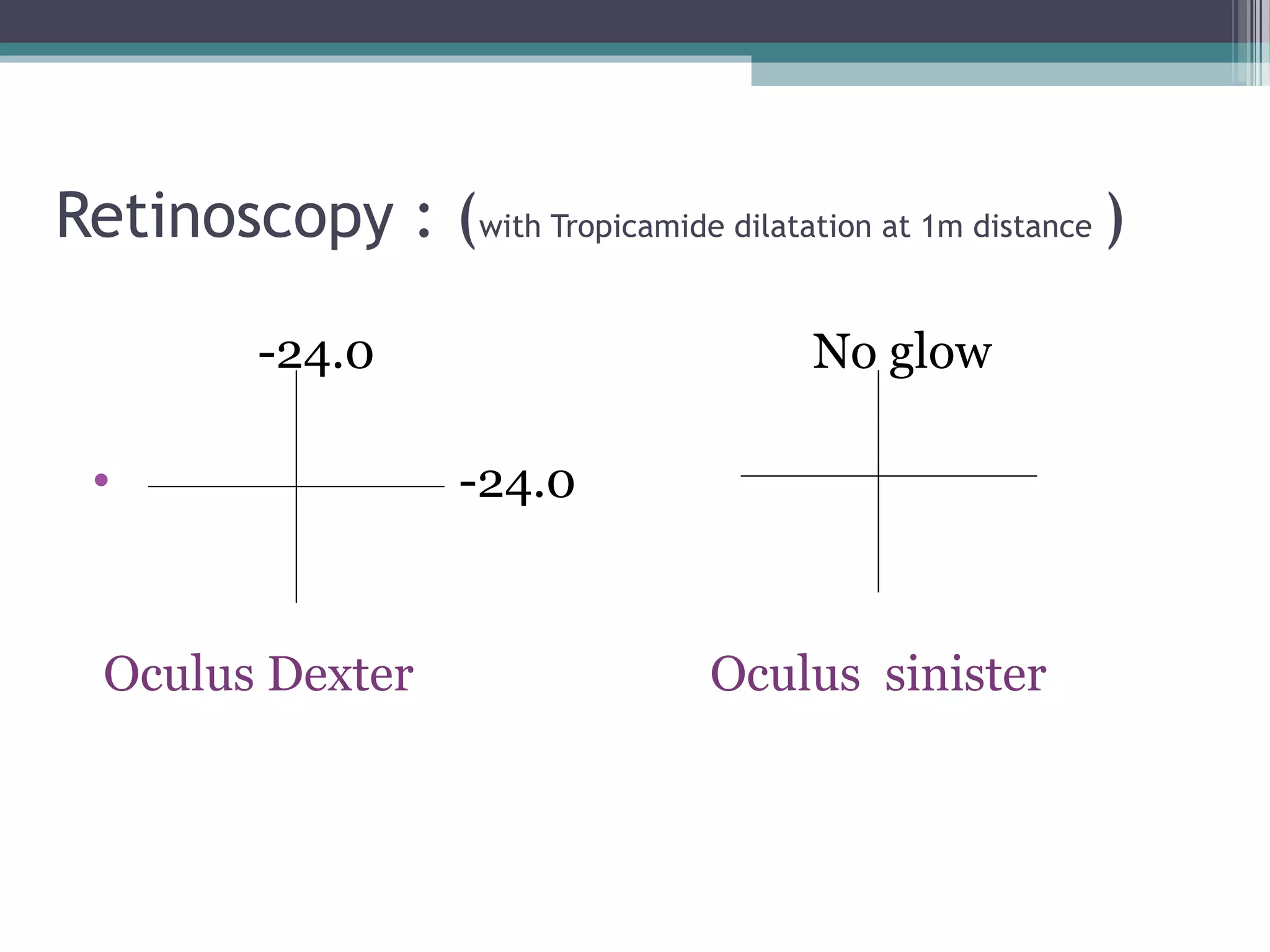
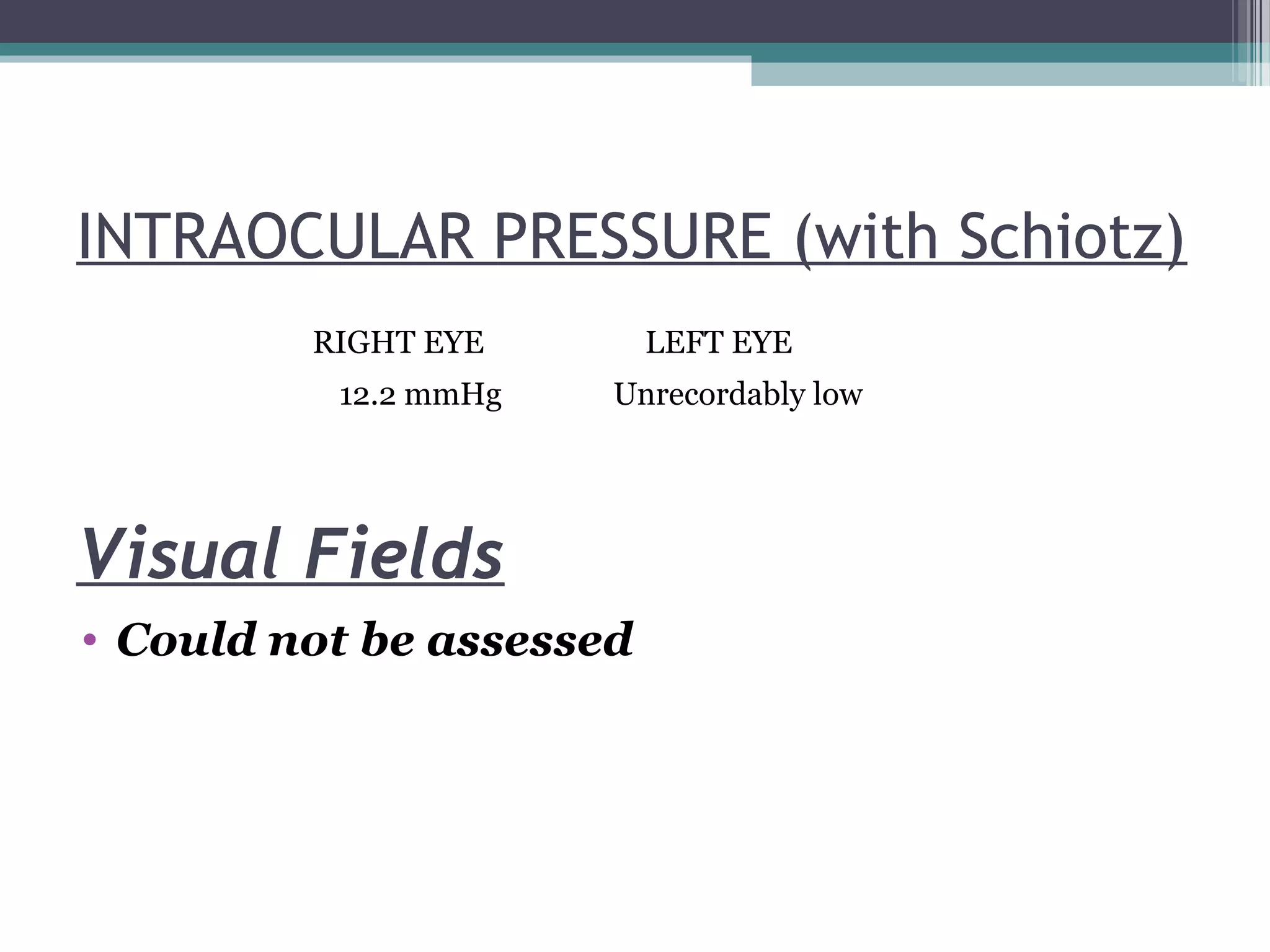
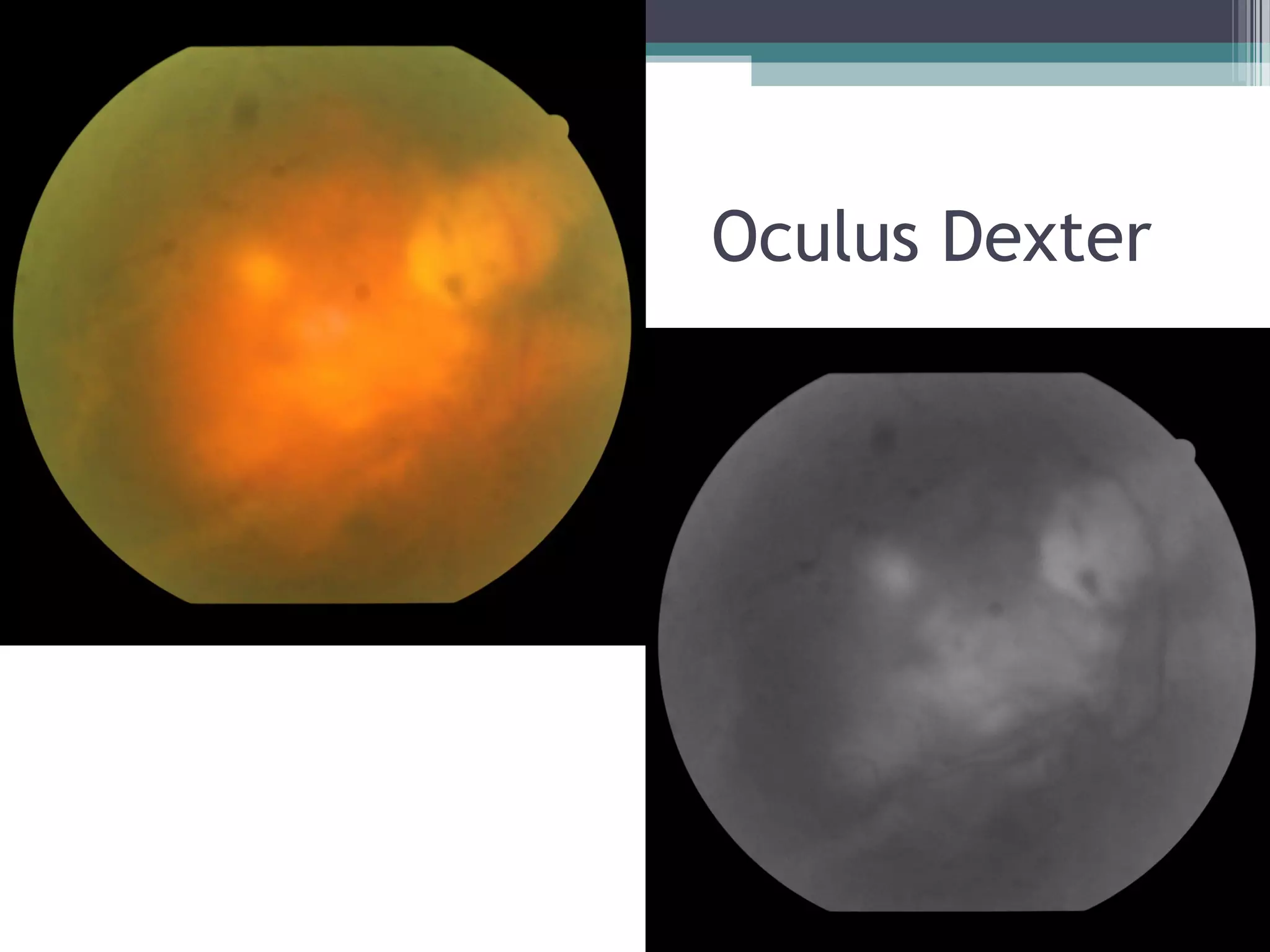
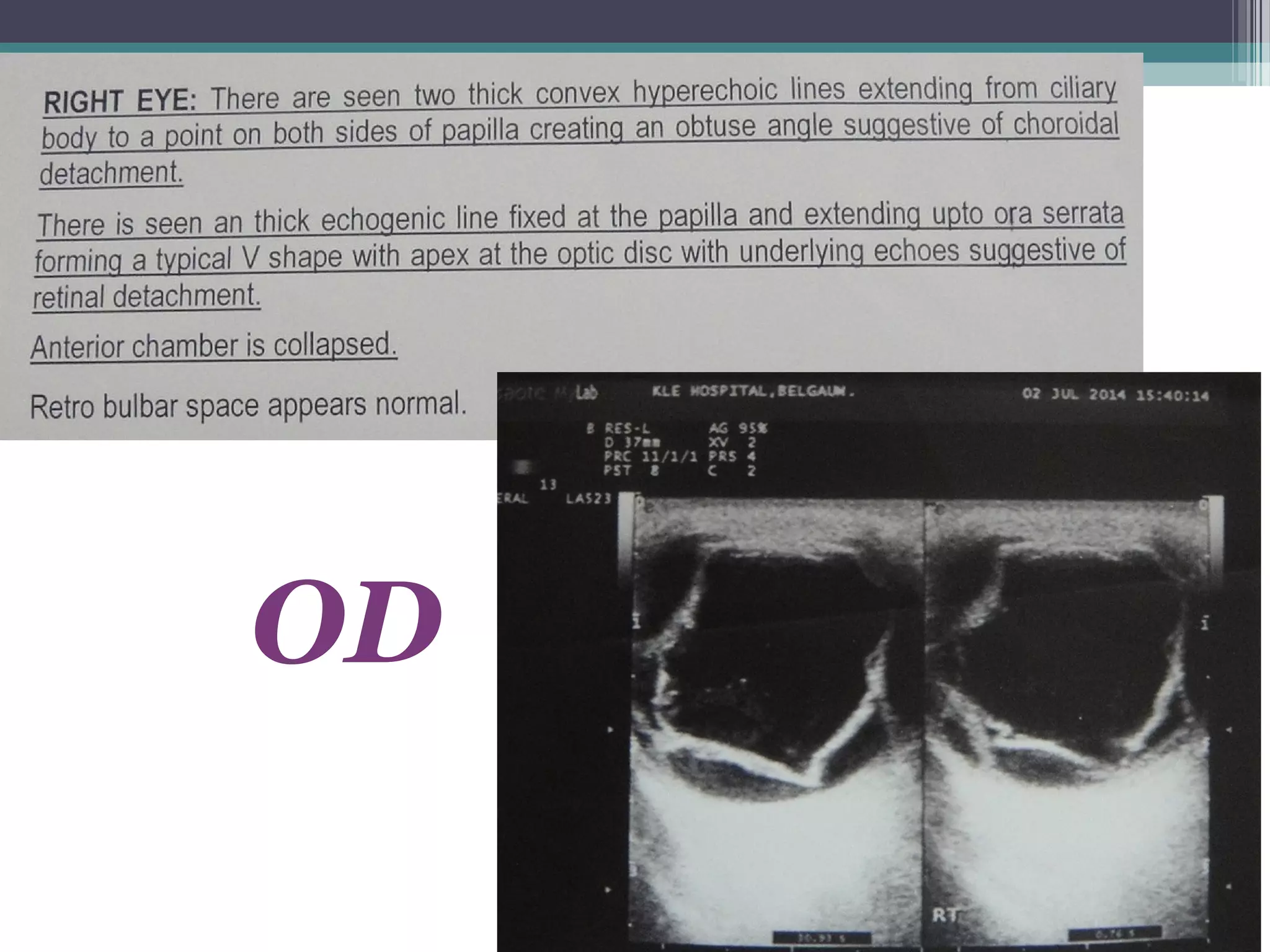
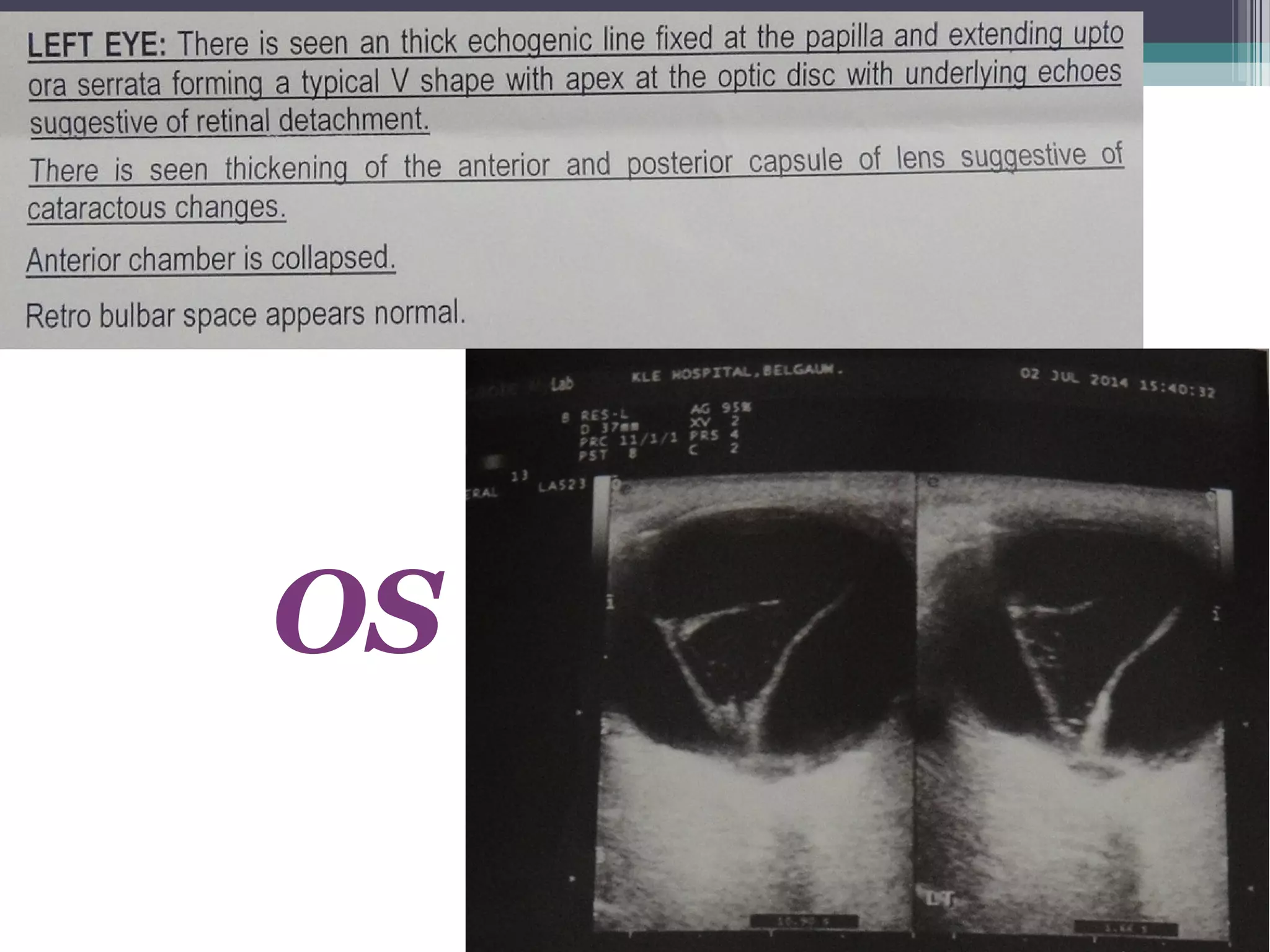
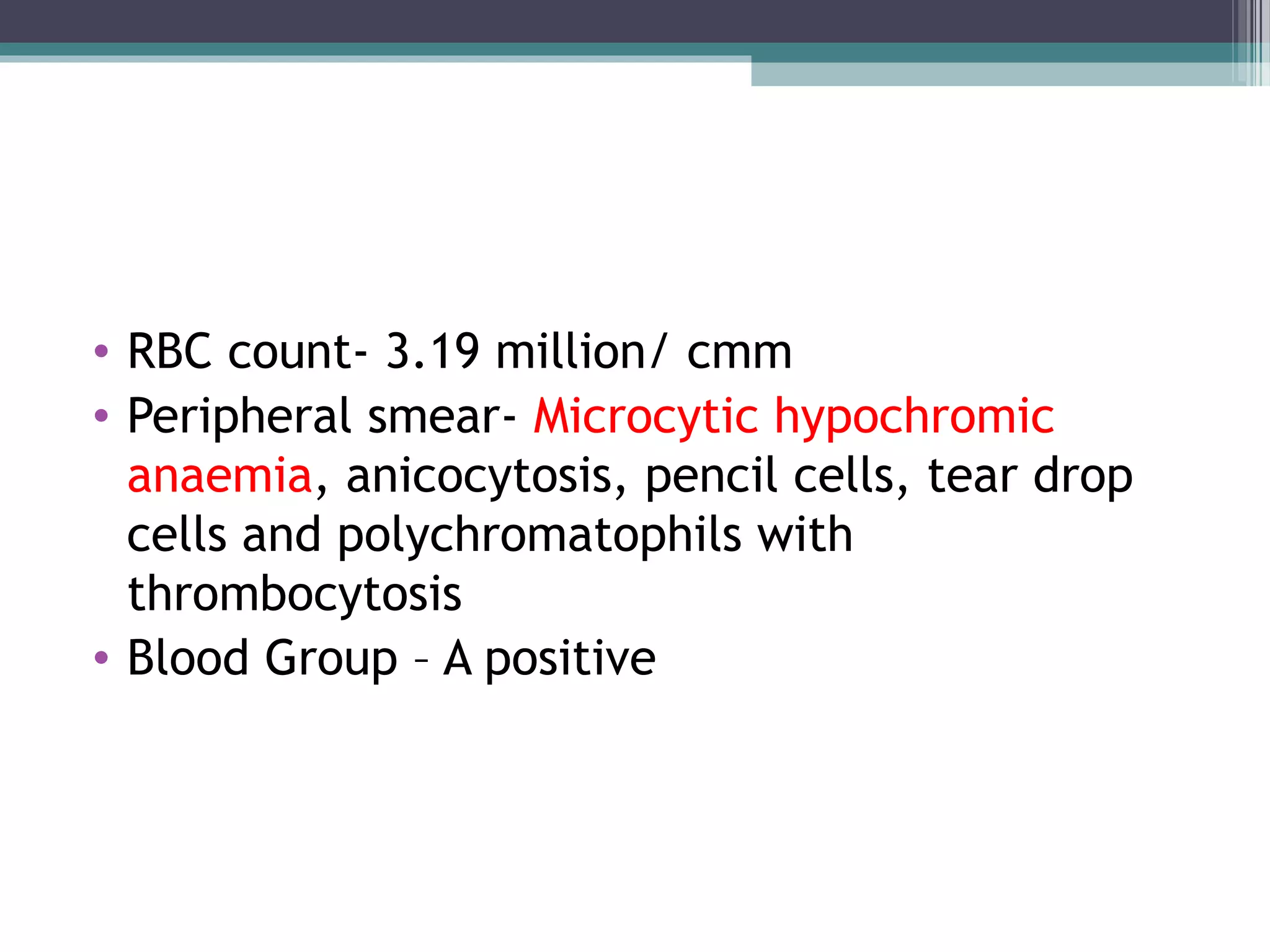
- A 50-year-old male presented with progressively diminishing vision in both eyes since childhood and sudden loss of vision in the right eye 20 days ago. Examination found high myopia, retinal detachment in the right eye, and mature cataract with total retinal detachment in the left eye. Investigations showed anemia. The patient was diagnosed with pathological myopia in both eyes, with retinal detachment in the right eye and cataract with retinal detachment in the left eye.