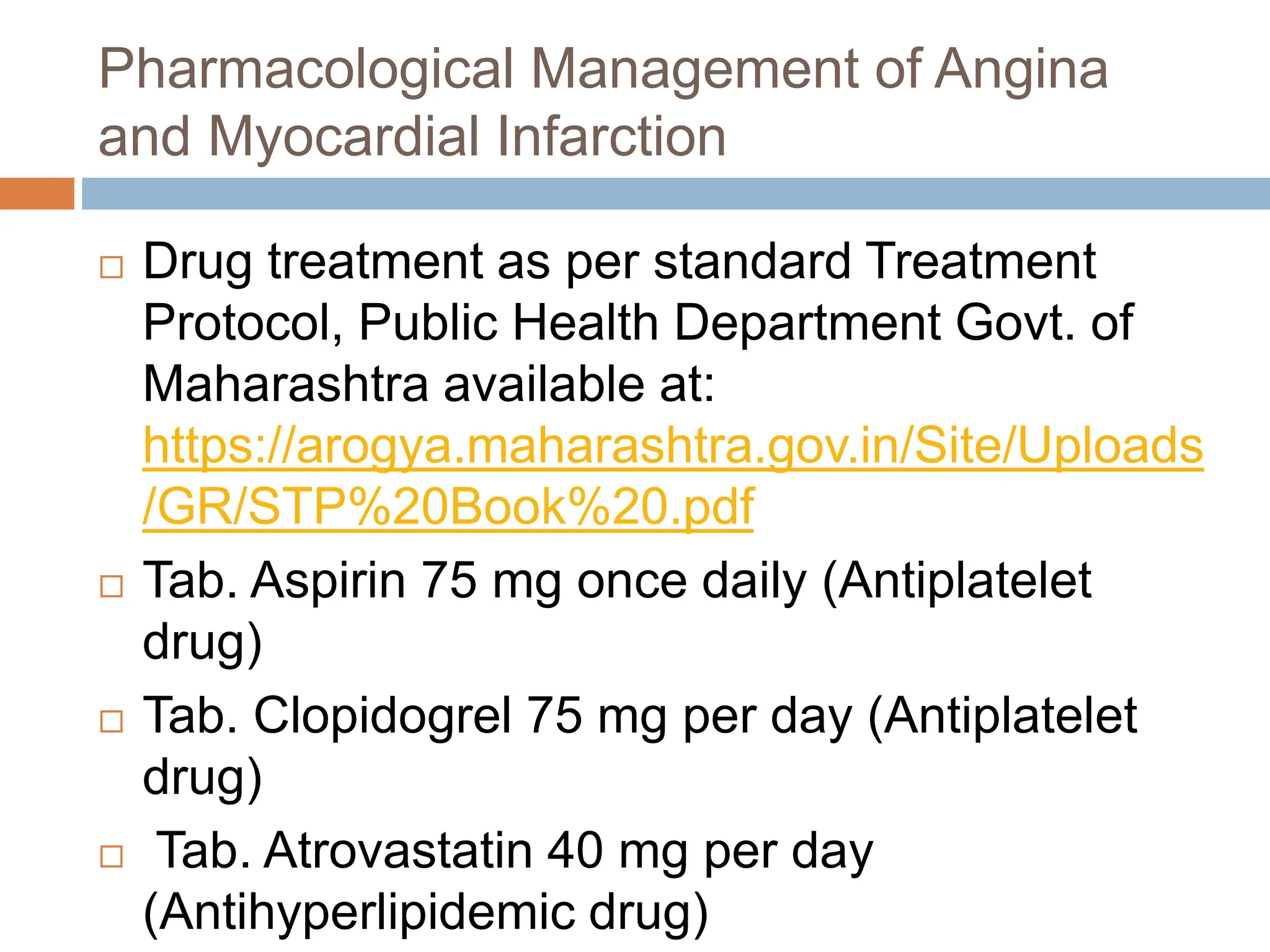
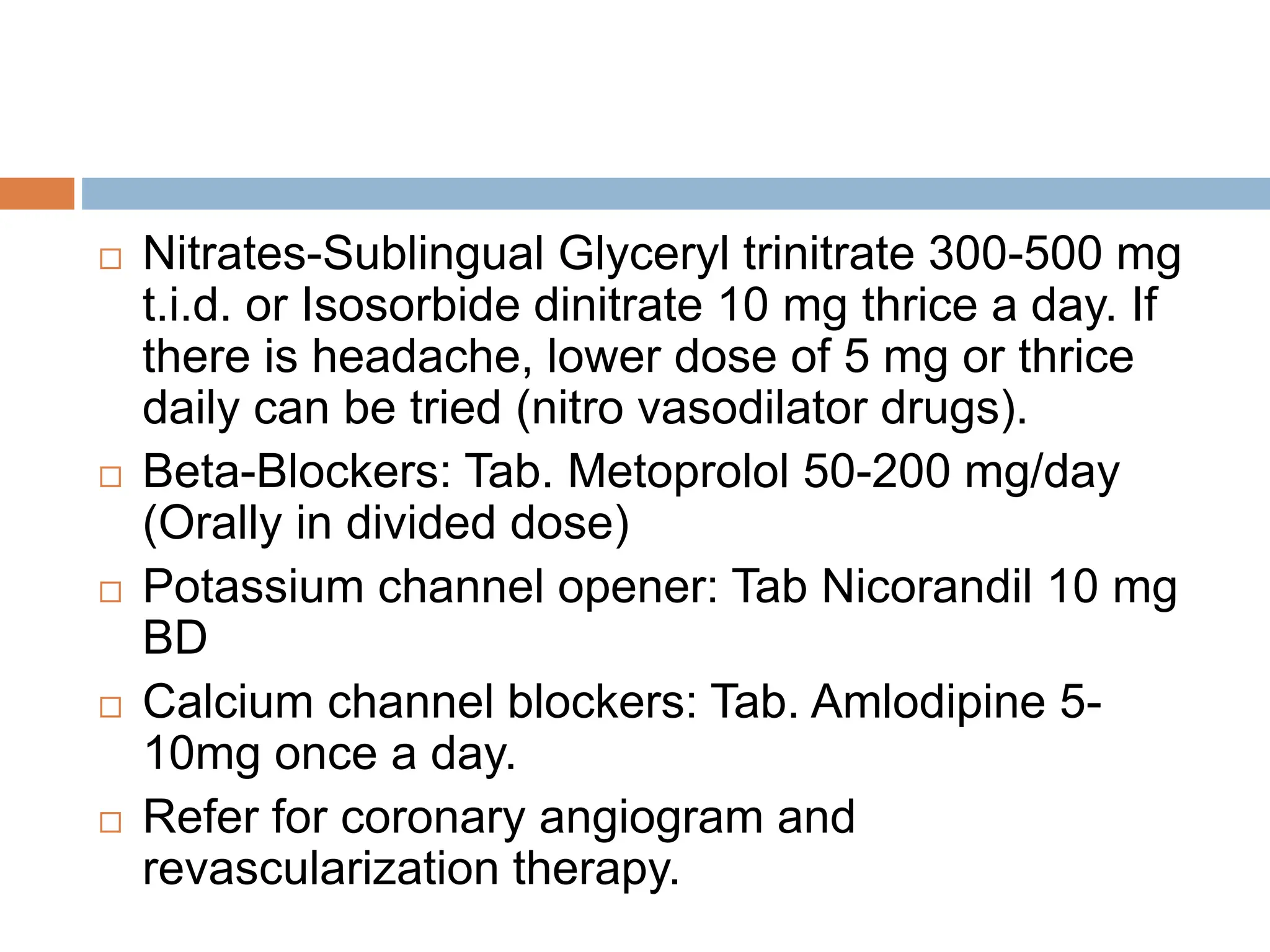
The document discusses cardiovascular diseases including hypertension, angina, myocardial infarction, and hyperlipidemia. It defines each condition and discusses their etiology, pathogenesis, clinical manifestations, diagnosis, and management. The management of hypertension and ischemic heart diseases involves identifying and modifying risk factors through lifestyle changes and medications.