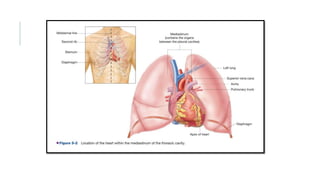
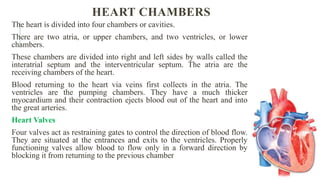
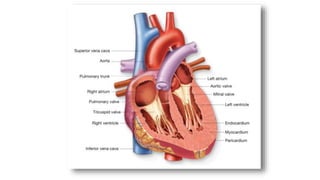
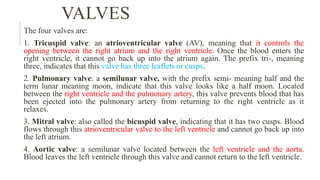
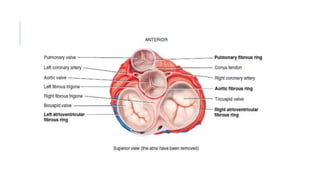
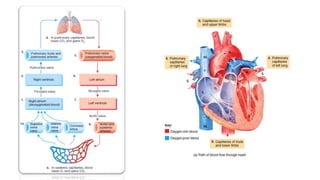
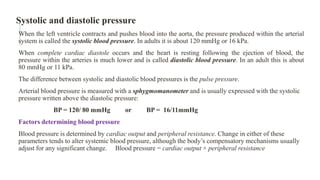
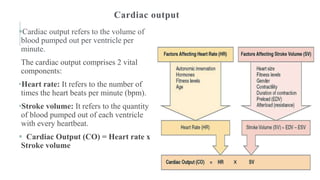
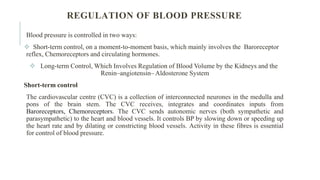
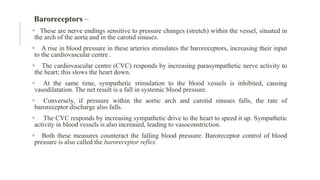
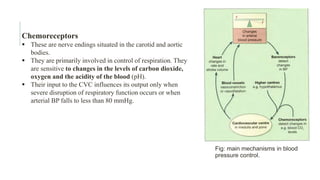
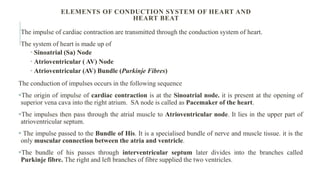
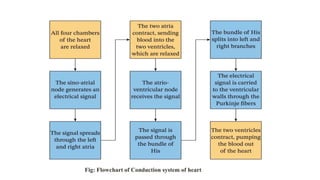
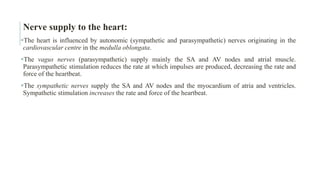
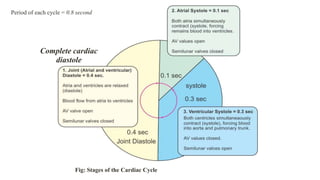
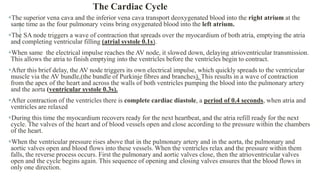
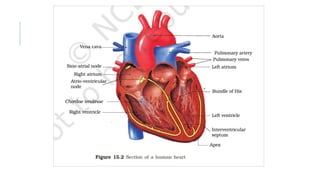
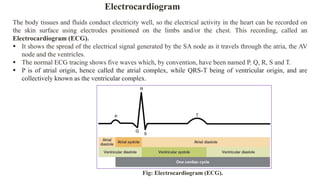
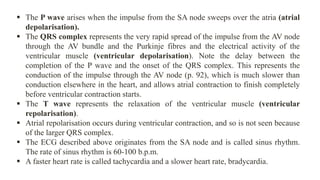
The document provides a detailed overview of the cardiovascular system, focusing on the anatomy and functions of the heart, including its structure, chambers, valves, and the processes of blood circulation and pressure regulation. It describes the heart's cardiac cycle, electrical conduction system, autonomic control of heart rate, and the significance of measuring blood pressure. Additionally, it explains the electrocardiogram (ECG) as a tool for monitoring heart activity.