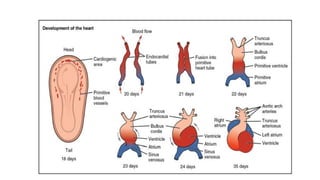
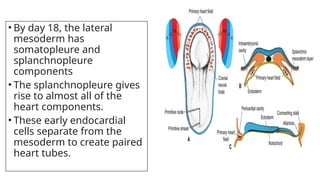
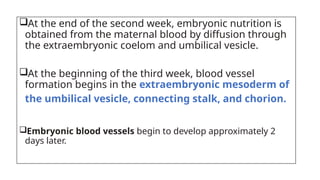
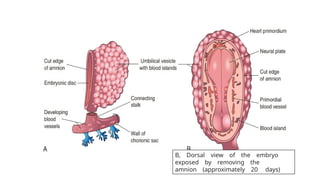
The document details the development of the heart and cardiovascular system in an embryo, highlighting the formation of the heart tubes, their fusion into a primordial heart tube, and the subsequent partitioning of the heart chambers. It describes critical stages of heart development, including the role of mesoderm, the formation of the cardiac loop, and the emergence of major blood vessels such as the aortic arches. Additionally, the text covers the embryonic nutrition process and the onset of blood circulation alongside the heart's functionality.