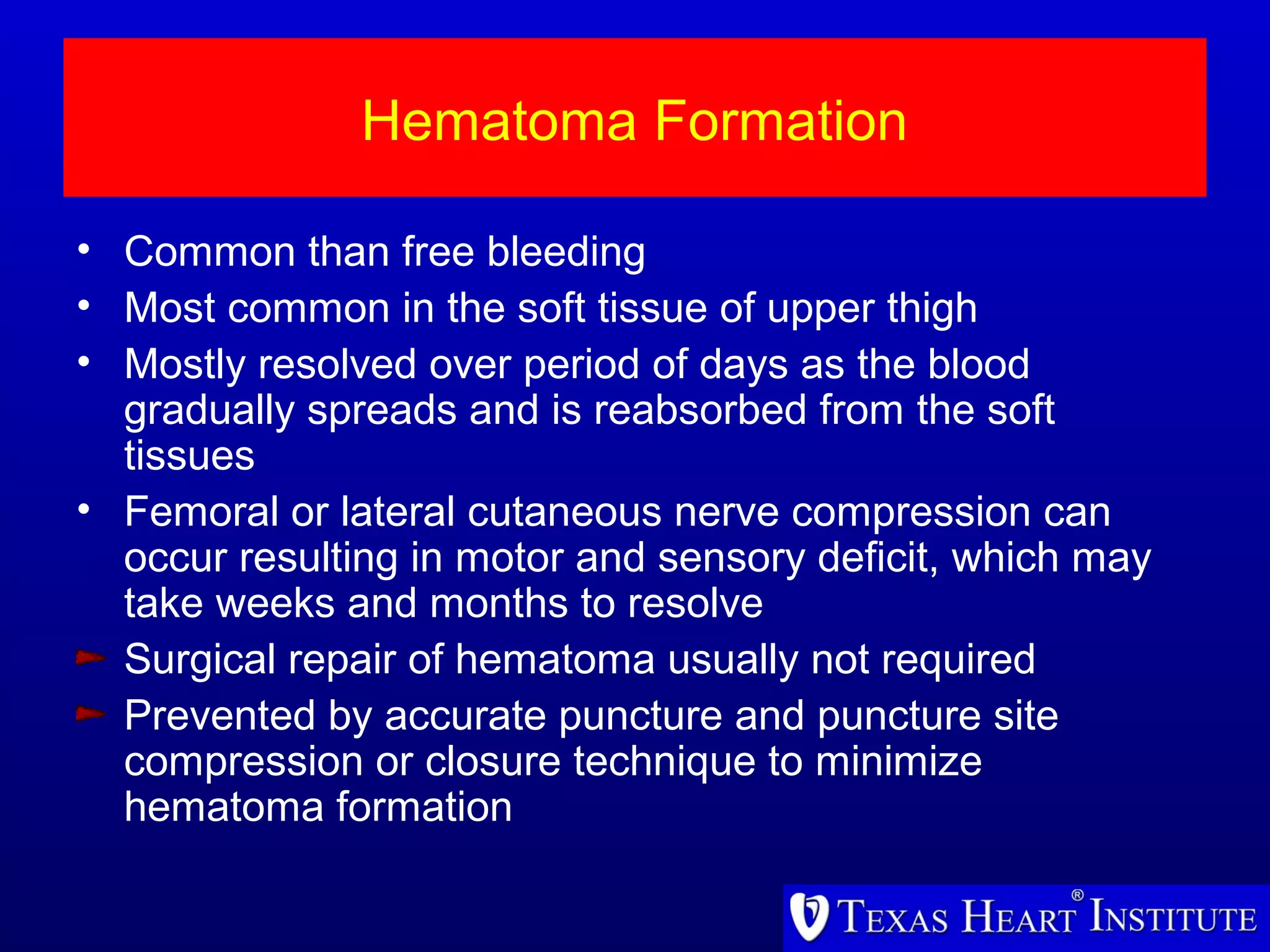
The document outlines the complications associated with cardiac catheterization, highlighting major risks such as death, myocardial infarction, stroke, and bleeding, with overall major complication rates being less than 1%. Factors affecting these risks include patient demographics, cardiovascular conditions, and the operator's experience. Local complications, including hematomas and pseudoaneurysms, are also discussed, along with the management strategies for these issues.