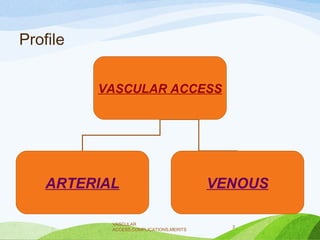
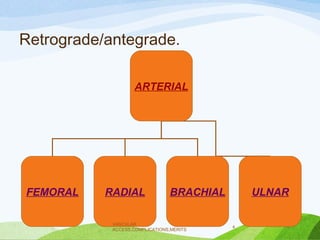
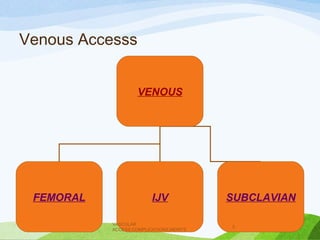
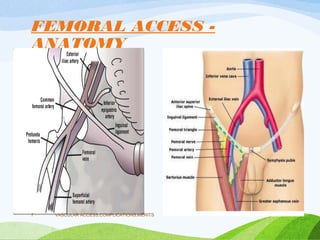
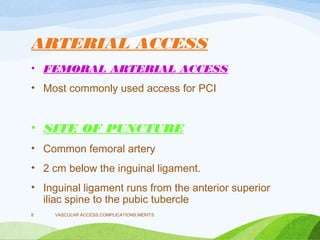
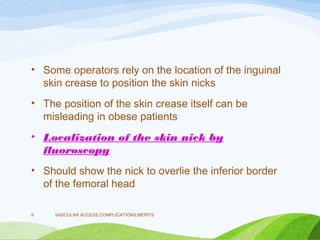
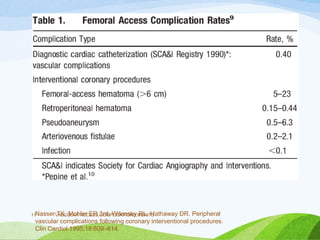
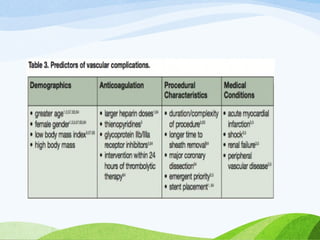
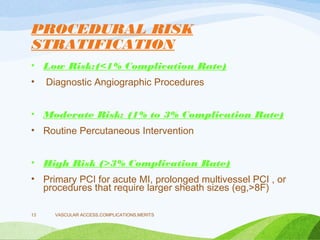
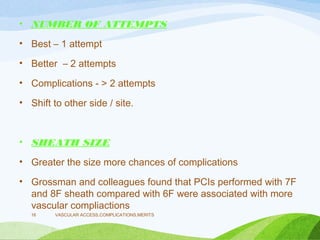
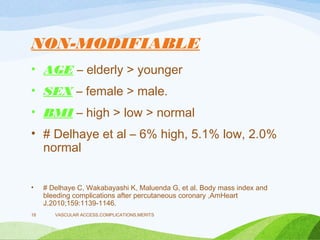
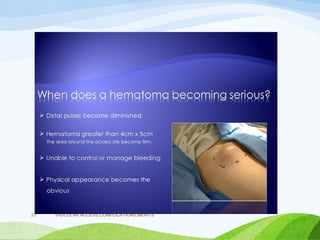
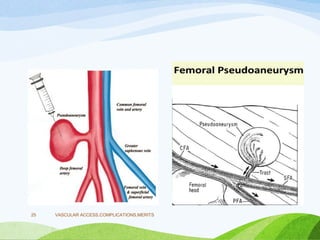
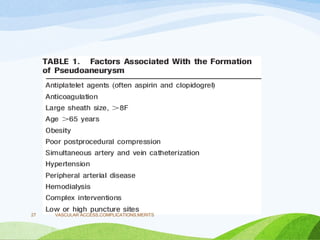
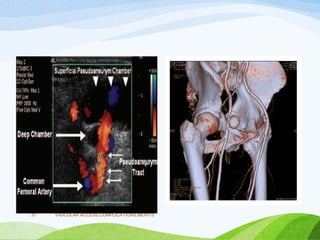
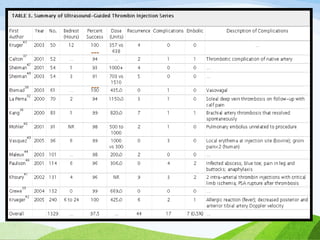
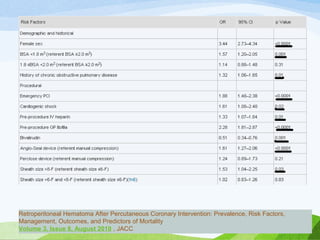
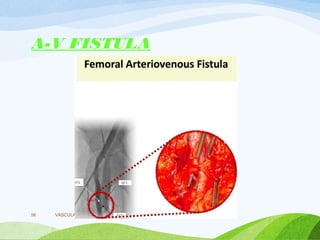
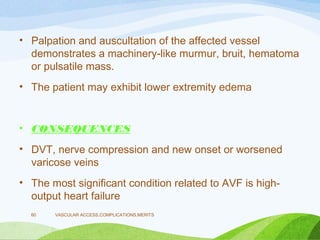
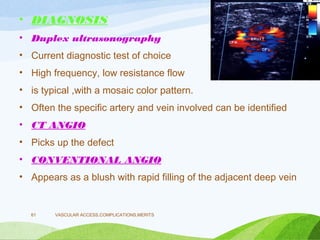
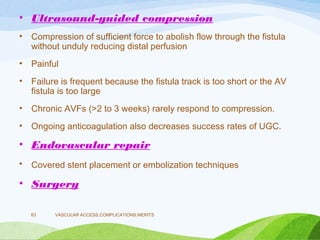
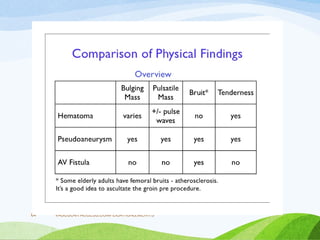
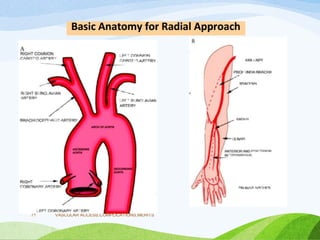
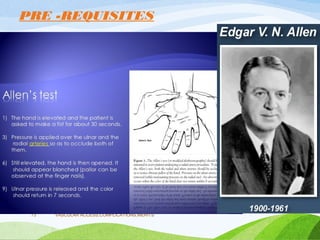
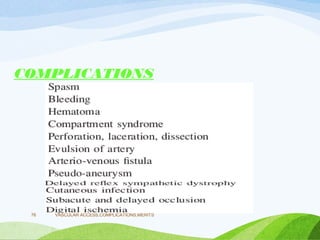
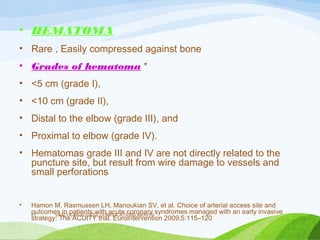
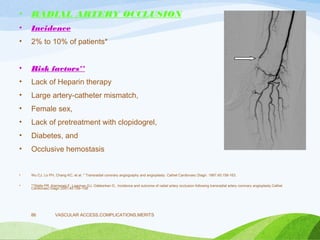
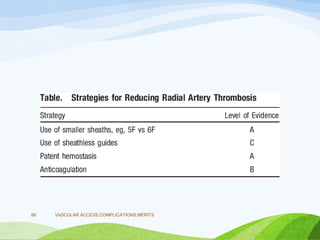
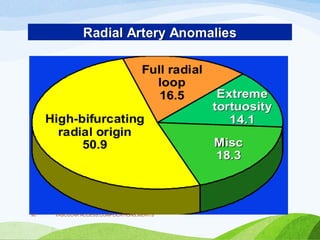
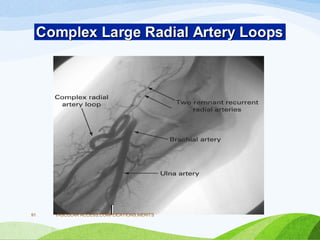
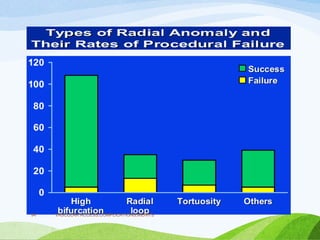
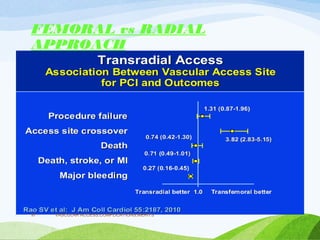
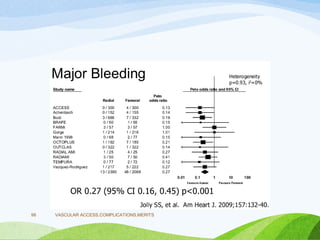
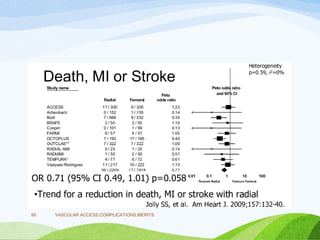
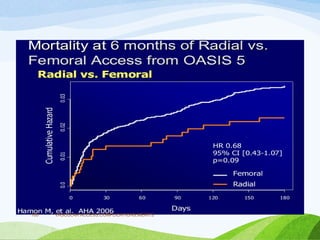
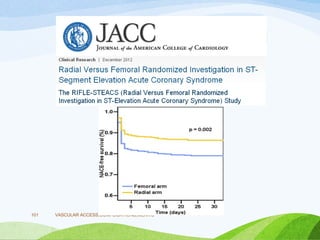
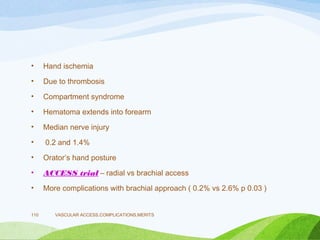
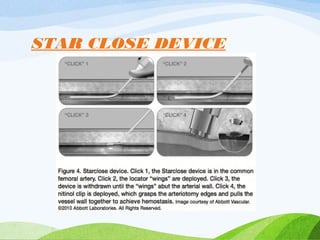
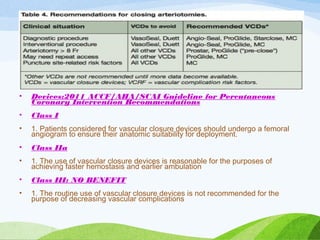
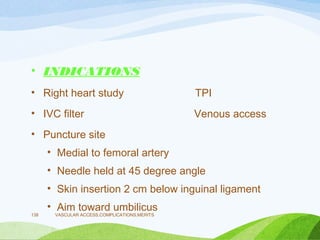
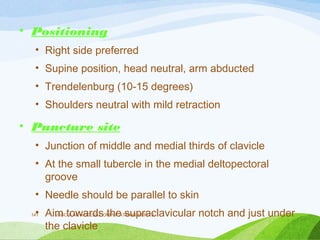
This document discusses vascular access during cardiac catheterization. It covers various topics related to arterial and venous access including common access sites, complications, risk factors, prevention of complications, and management of complications. Specific complications discussed in detail include hematoma, pseudoaneurysm, retroperitoneal hemorrhage. Treatment options for complications like ultrasound-guided compression, thrombin injection, endoluminal techniques are also summarized.