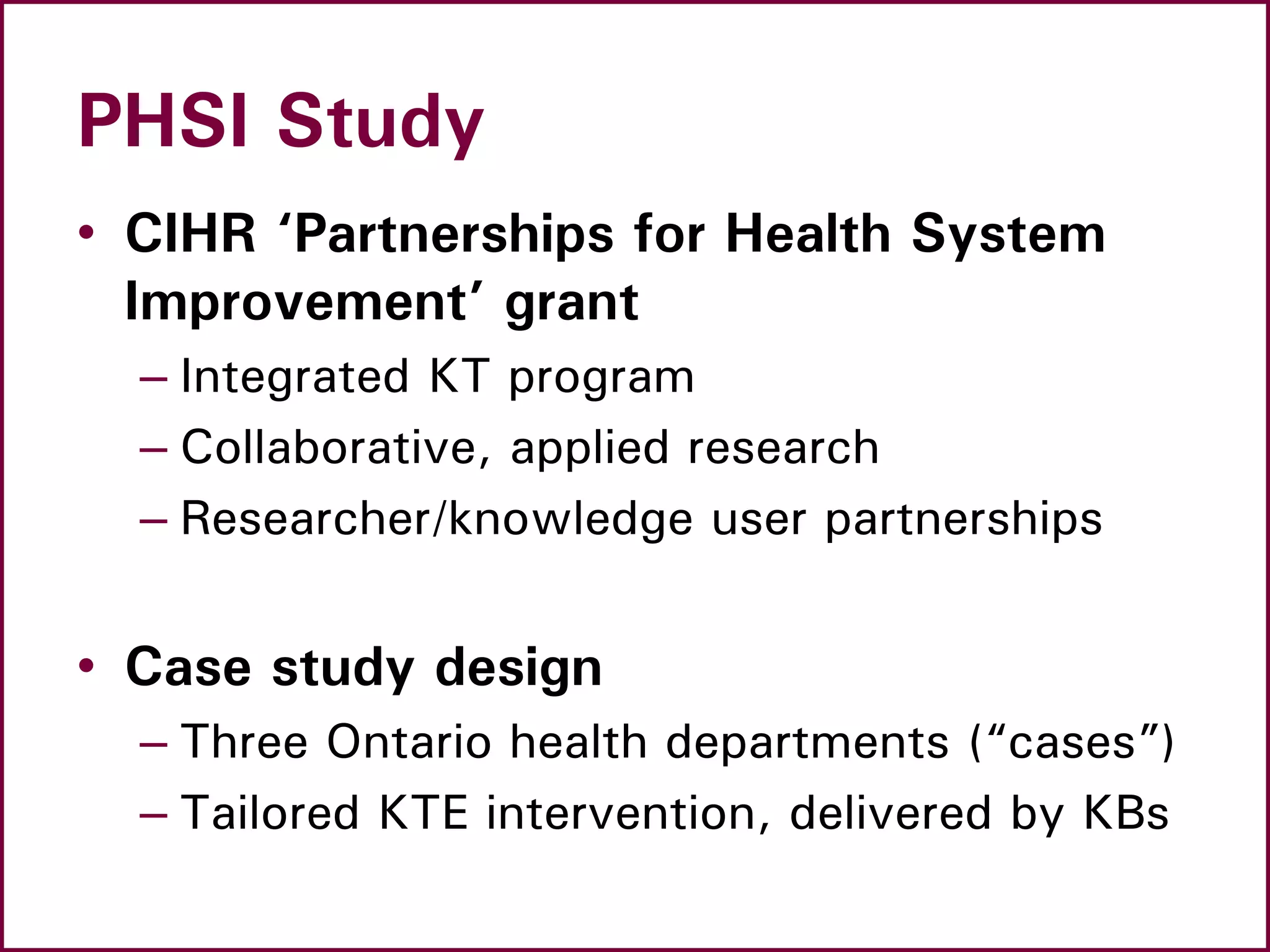
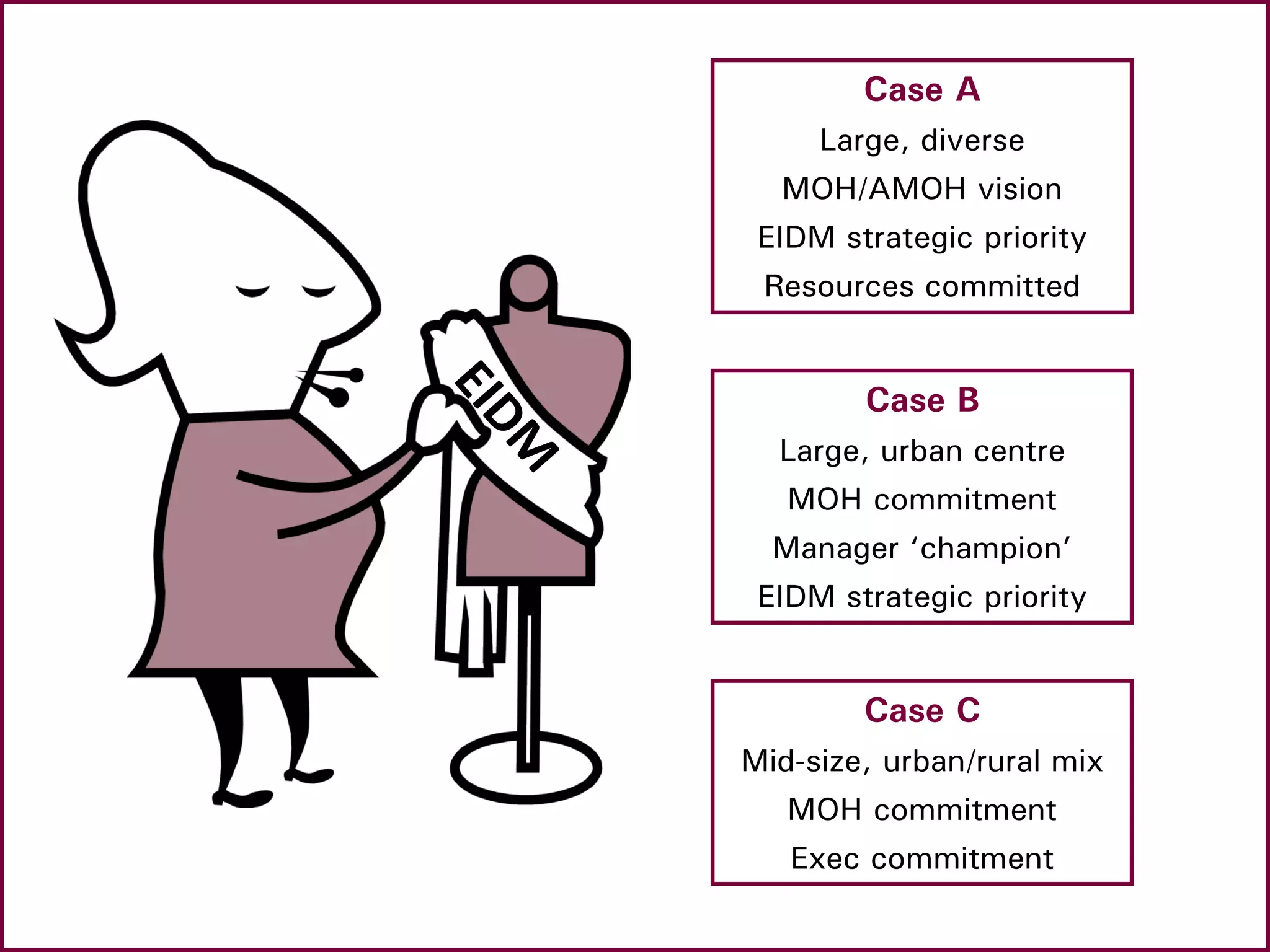
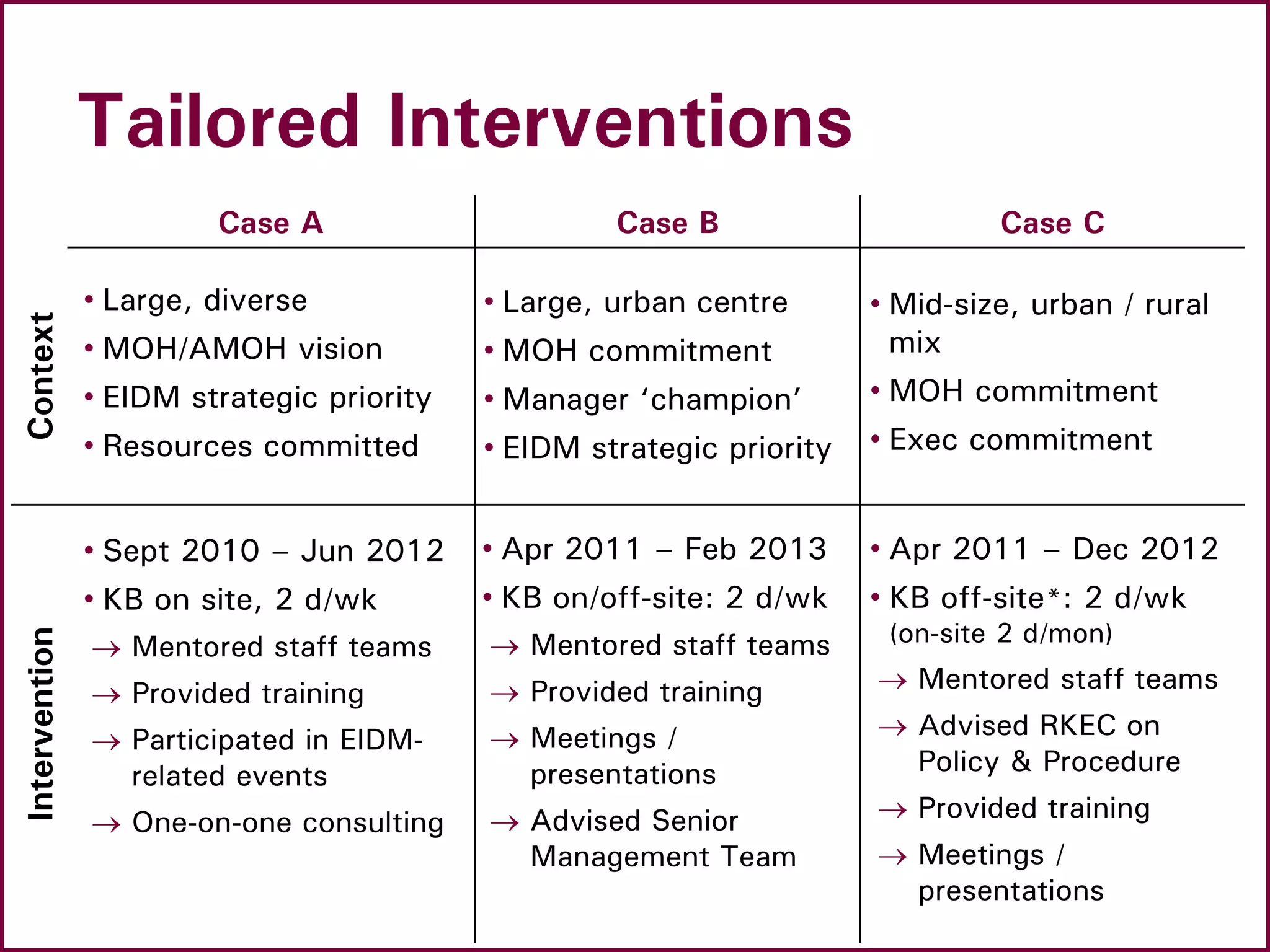
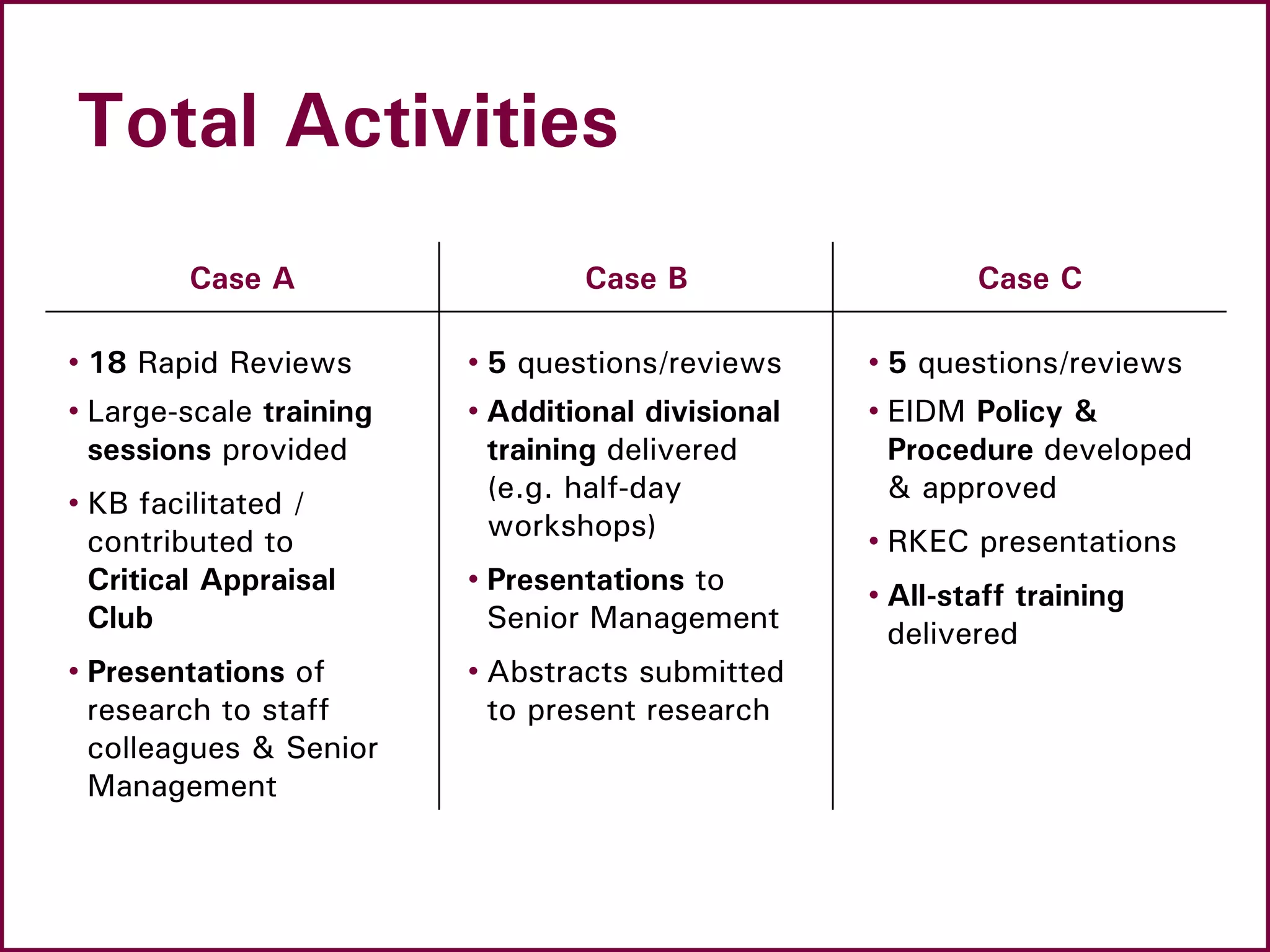
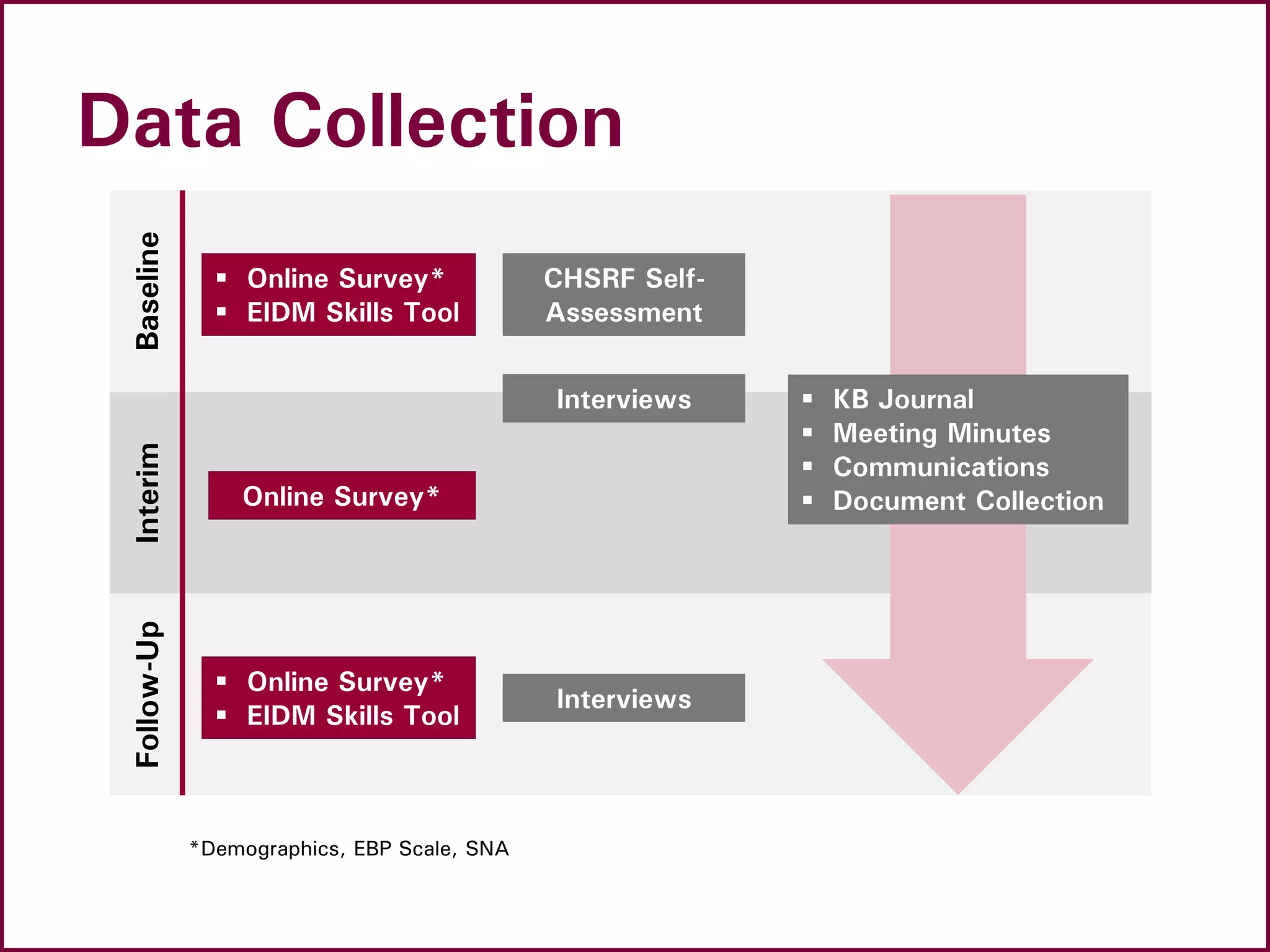
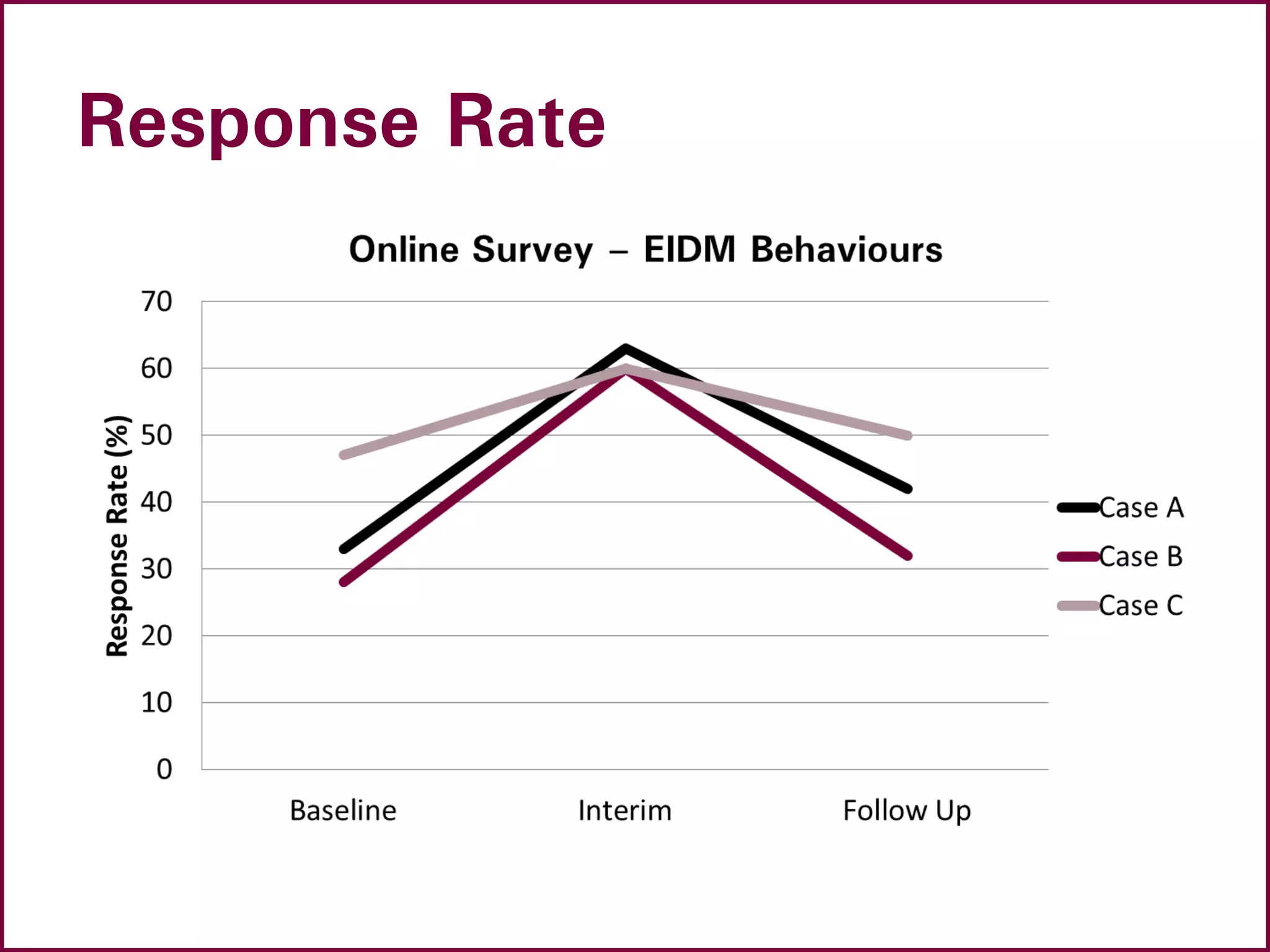
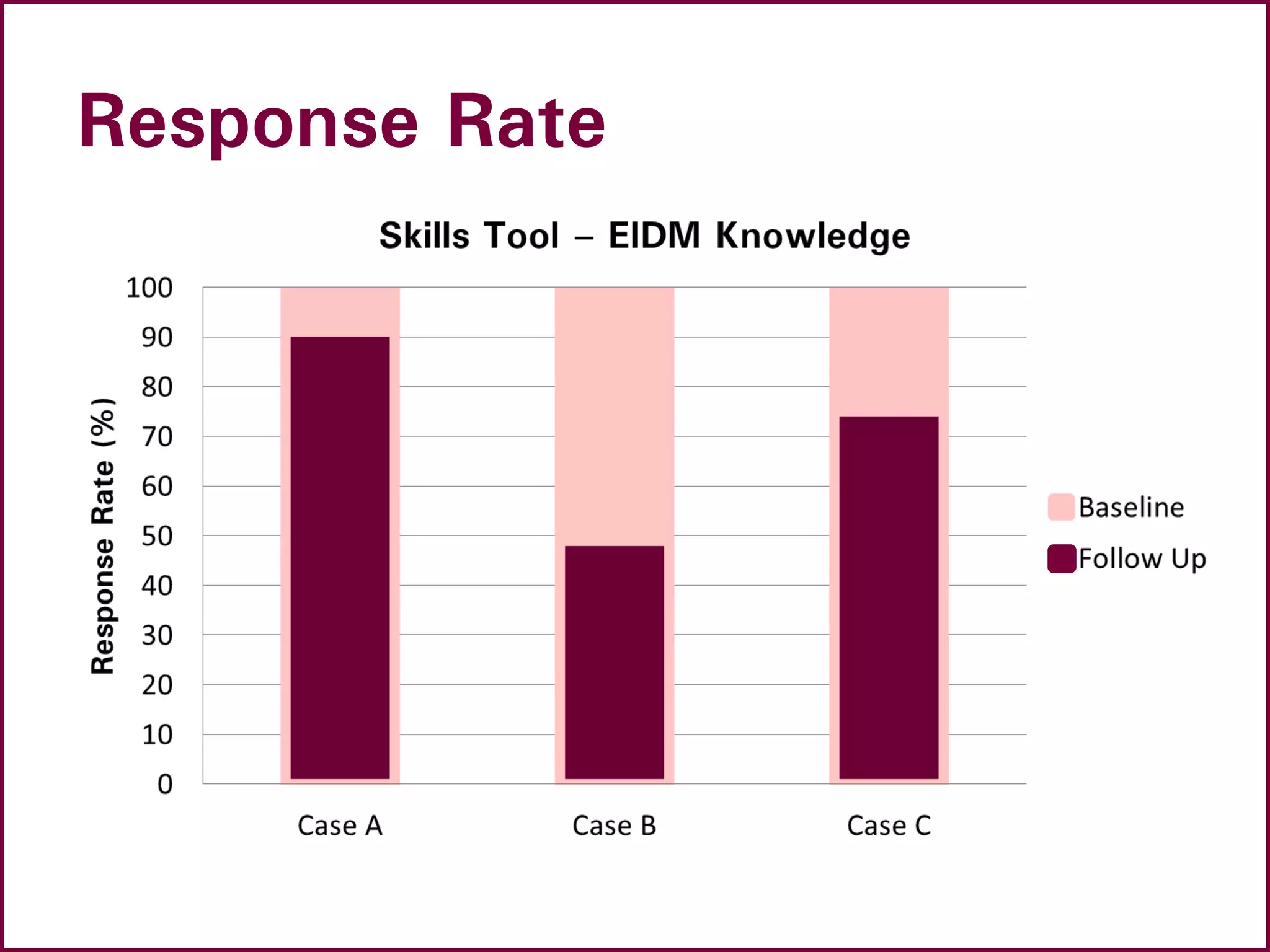
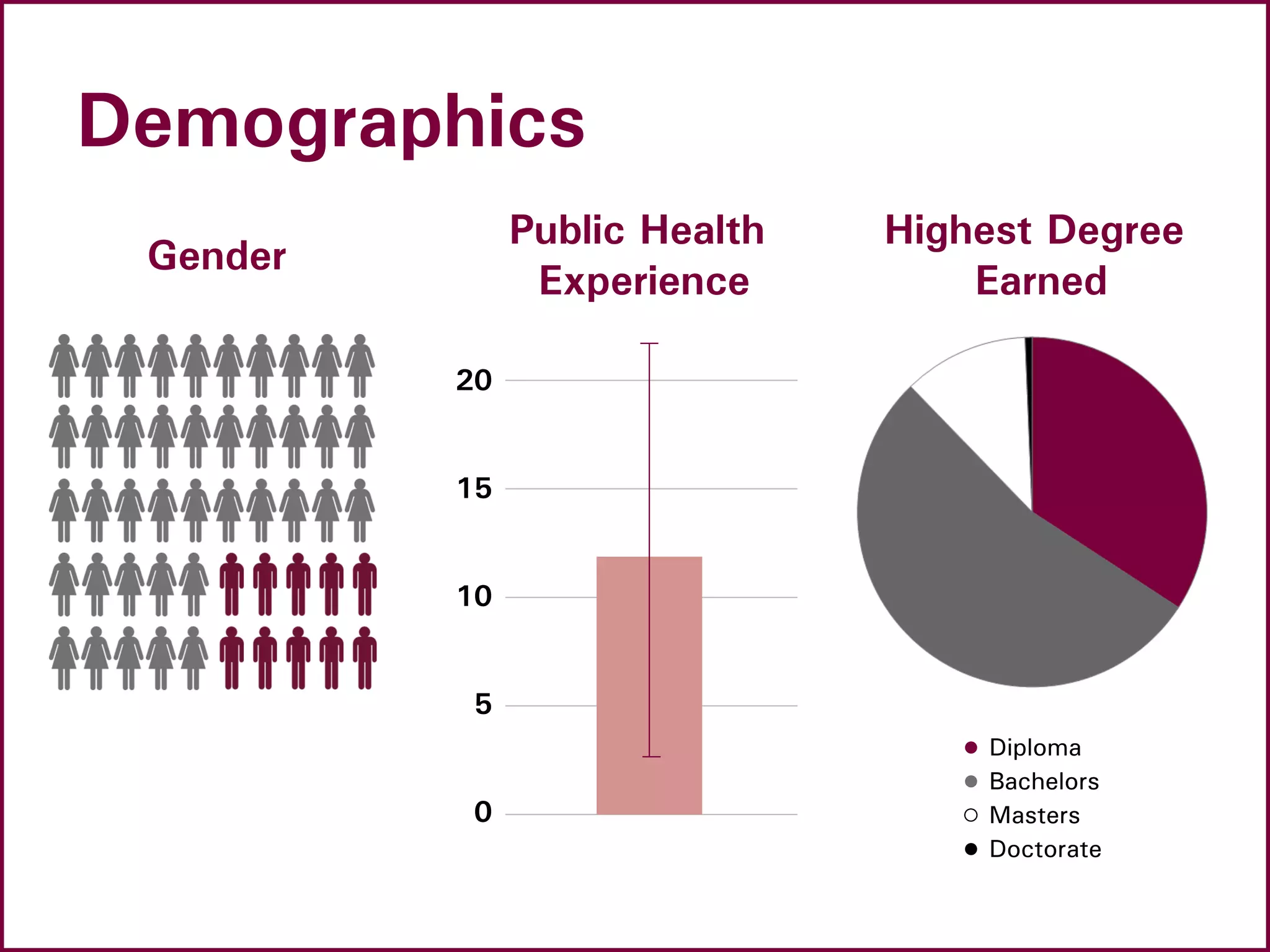
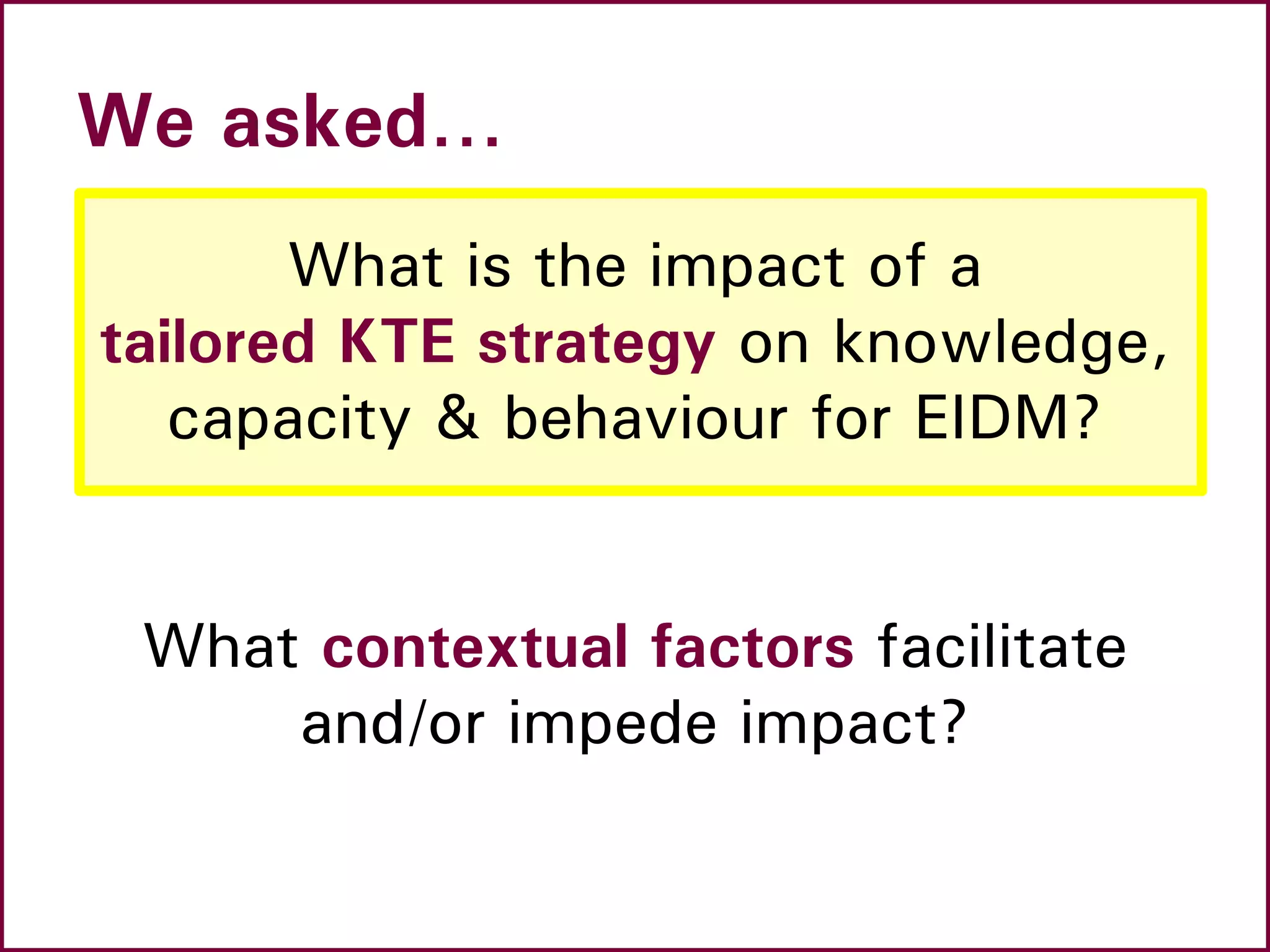
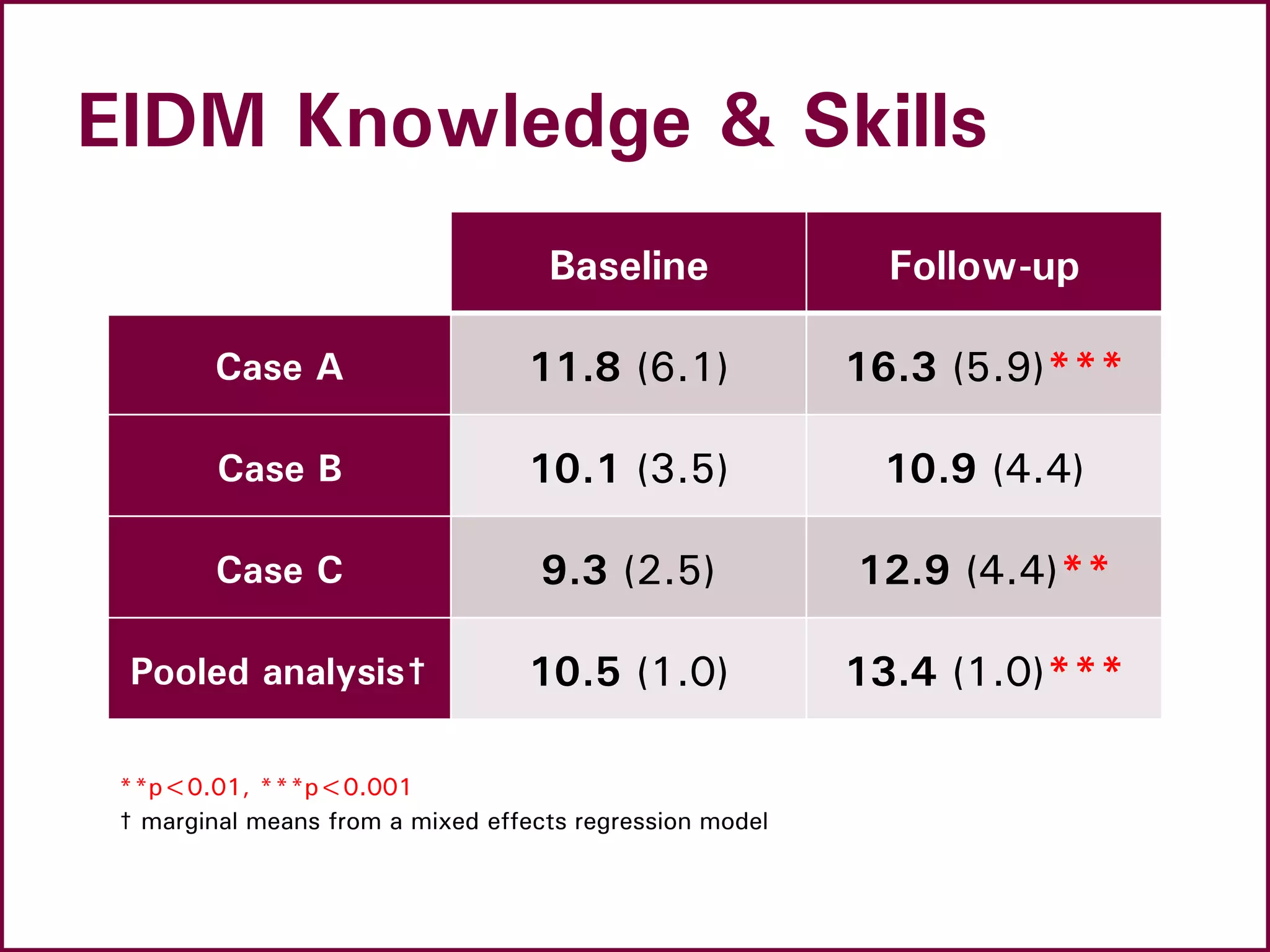
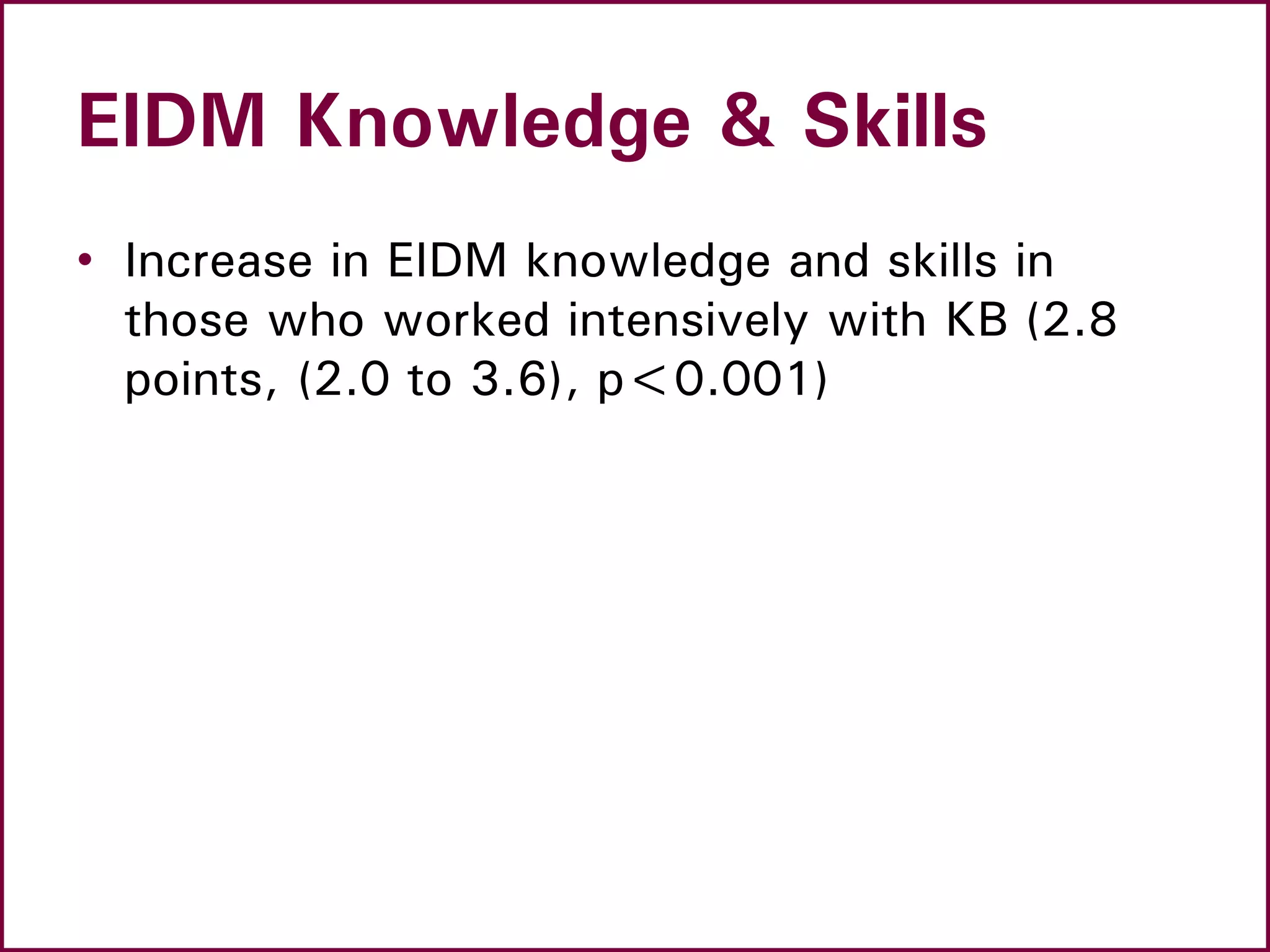
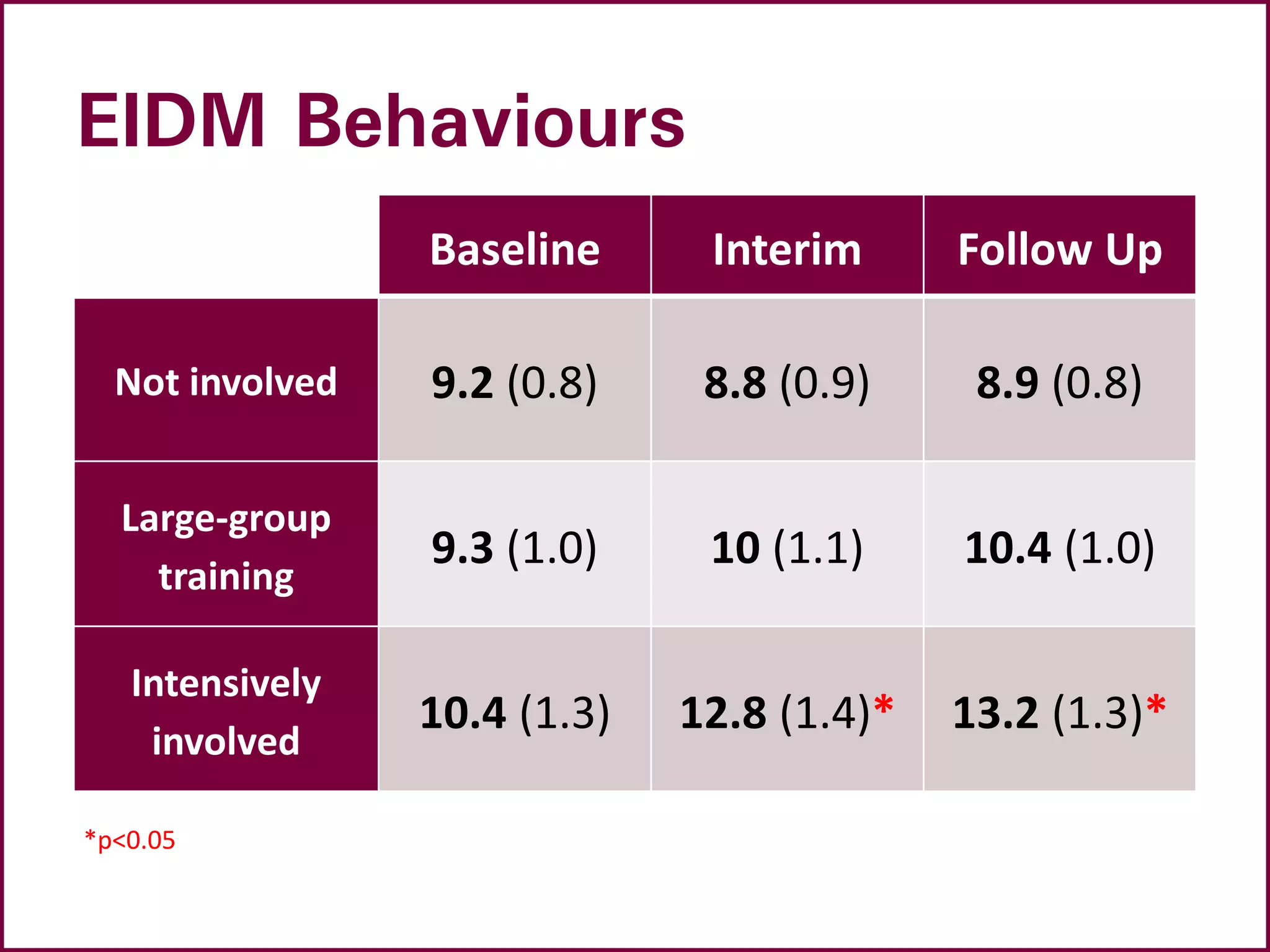
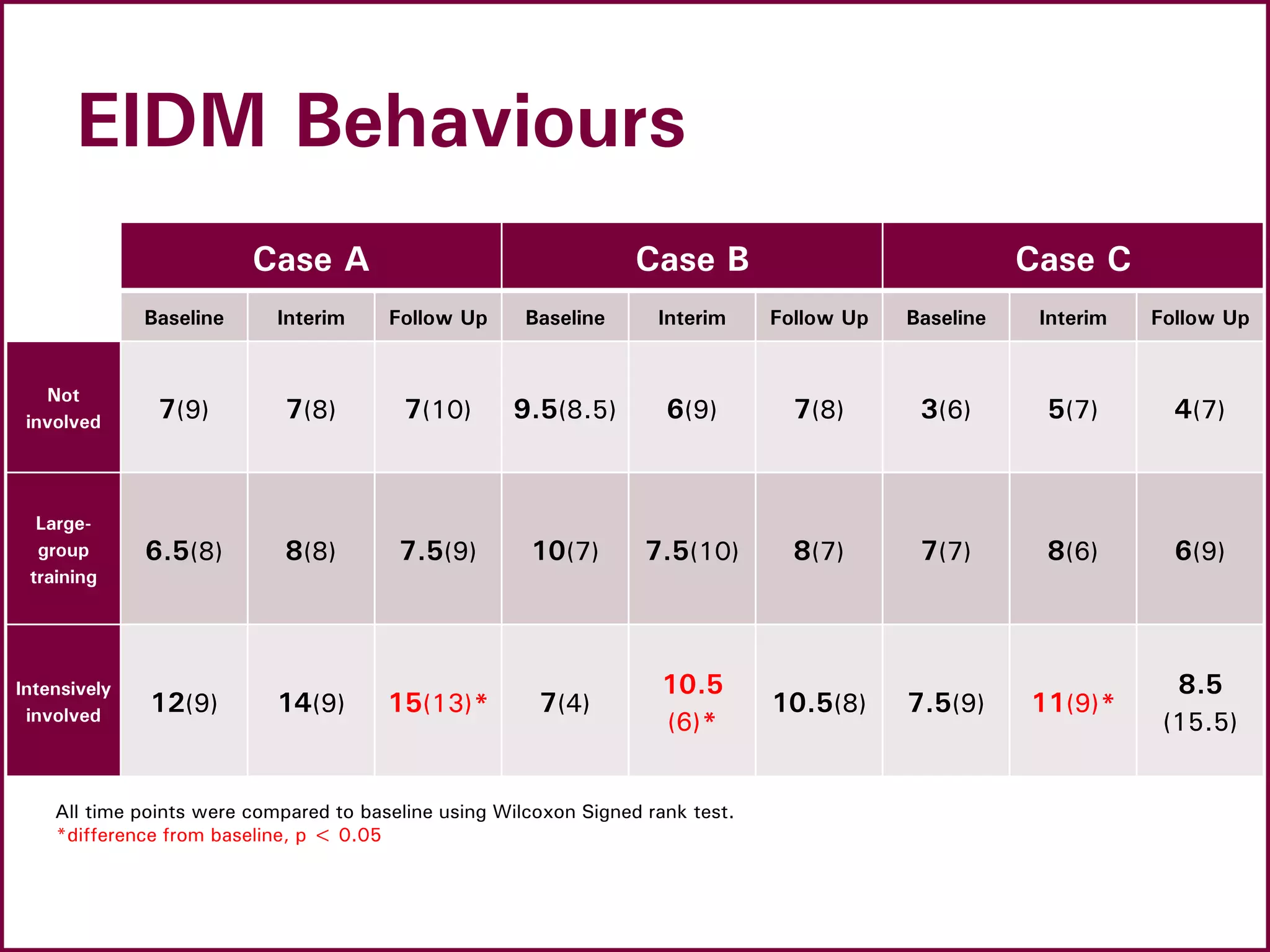
The document outlines a webinar on building capacity for evidence-informed public health decision-making, discussing tailored knowledge translation and exchange strategies used in three Ontario health departments. Key findings indicate that public health practitioners who engaged closely with knowledge brokers showed significant improvements in their knowledge, skills, and behaviors related to evidence-informed decision-making. The webinar highlights both the benefits and challenges of implementing these strategies in public health contexts.

![A Model for Evidence-Informed
Decision Making
National Collaborating Centre for Methods and Tools. (revised 2012).
A Model for Evidence-Informed Decision-Making in Public Health (Fact
Sheet). [http://www.nccmt.ca/pubs/FactSheet_EIDM_EN_WEB.pdf]](https://image.slidesharecdn.com/healthevidencephsiresultswebinar10june2014-140611113625-phpapp01/75/Building-capacity-for-evidence-informed-public-health-decision-making-7-2048.jpg)
![Stages in the process of
Evidence-Informed Public Health
National Collaborating Centre for Methods and Tools. Evidence-
Informed Public Health. [http://www.nccmt.ca/eiph/index-eng.html]](https://image.slidesharecdn.com/healthevidencephsiresultswebinar10june2014-140611113625-phpapp01/75/Building-capacity-for-evidence-informed-public-health-decision-making-8-2048.jpg)