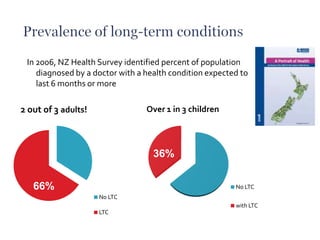
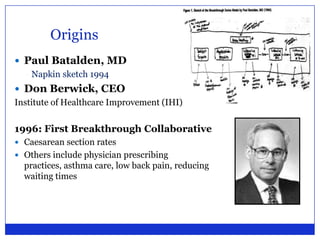
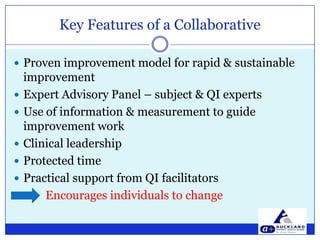
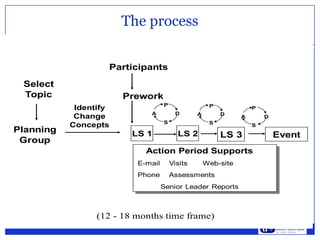
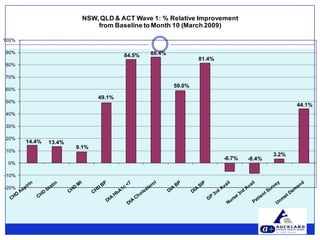
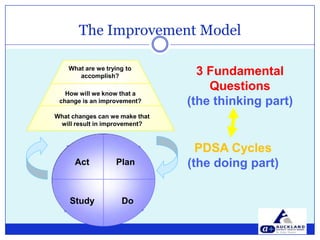
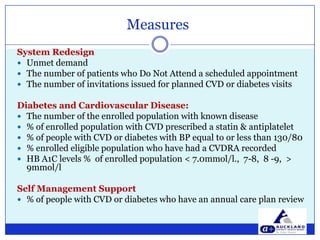
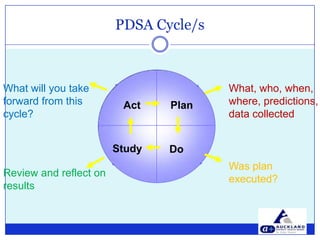
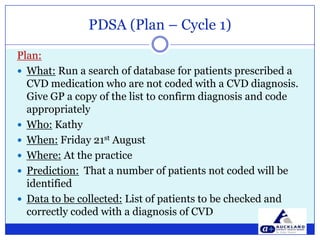
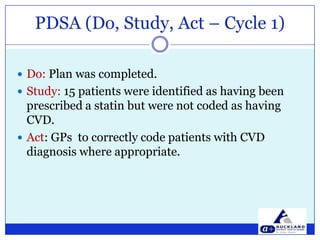
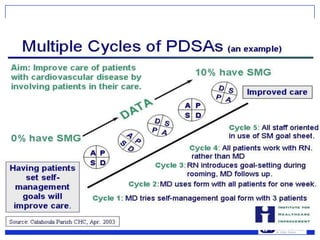
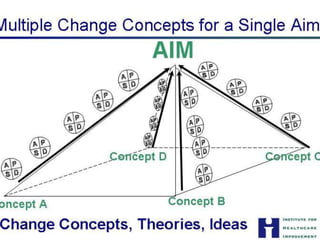
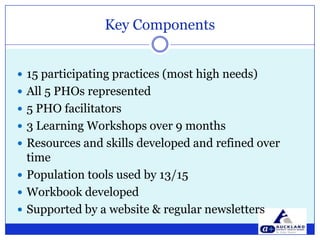
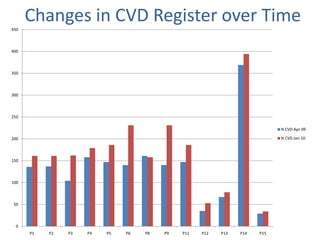
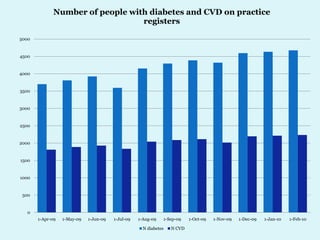
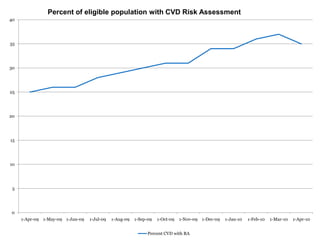
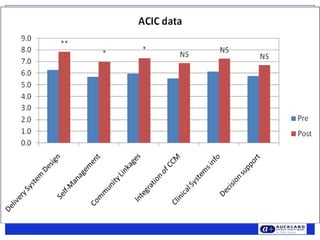
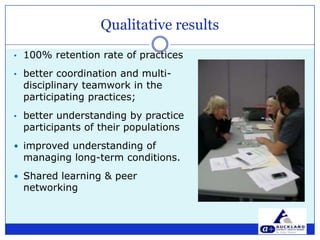
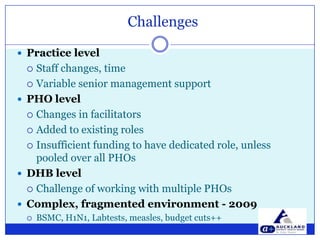
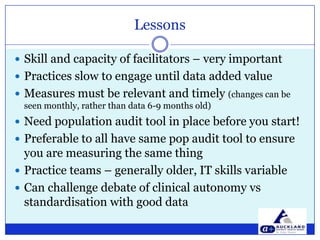
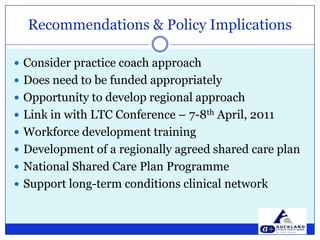
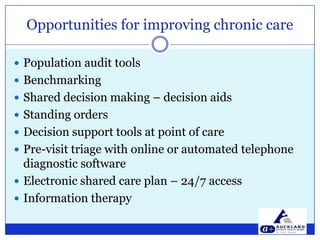
This document outlines a presentation on improving chronic care in New Zealand using a collaborative methodology within primary care. It discusses the prevalence of long-term conditions, the collaborative's characteristics, key outcomes, and experiences from participating practices. Challenges and recommendations for implementing quality improvement practices in the healthcare system are also highlighted.