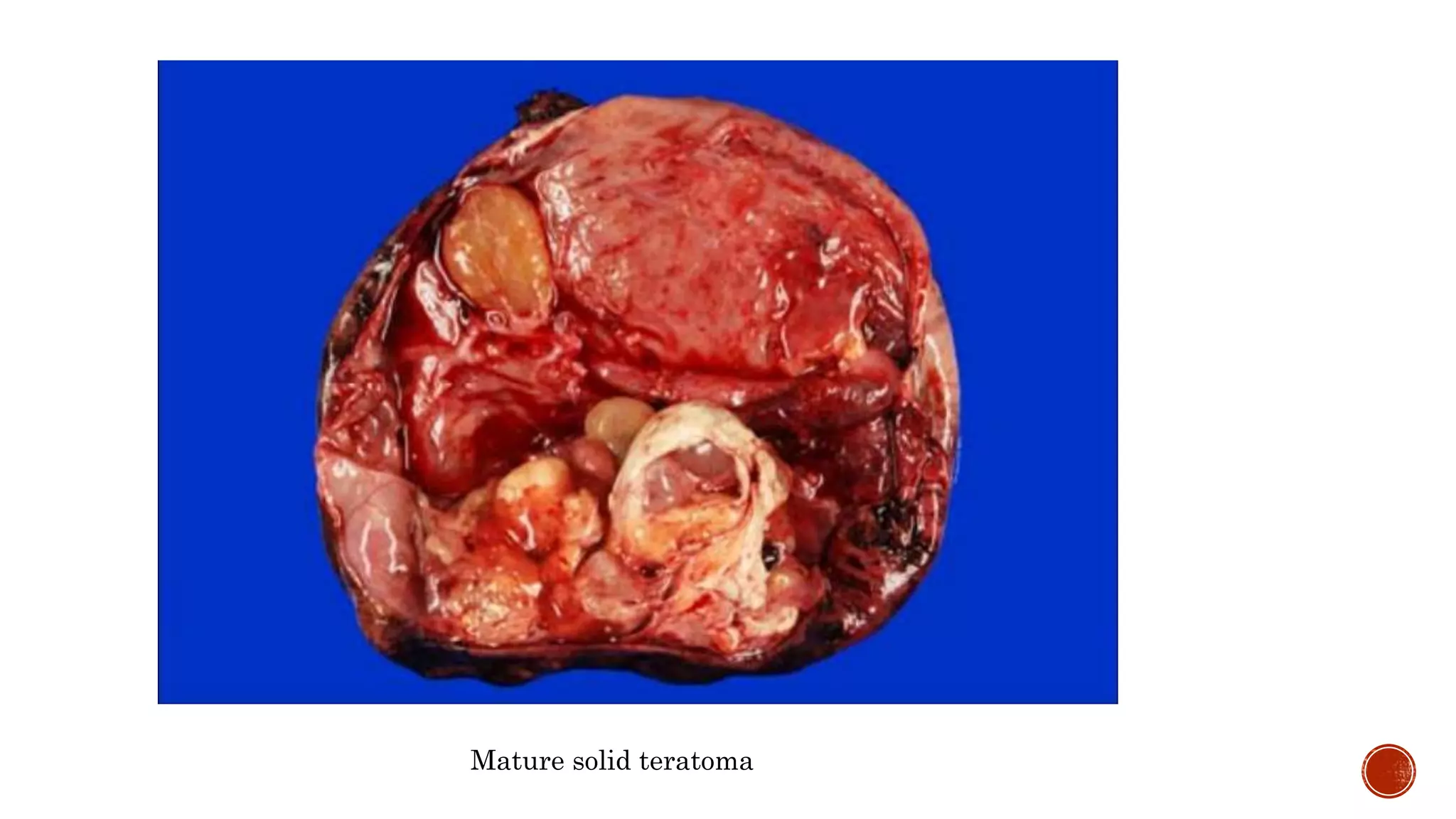
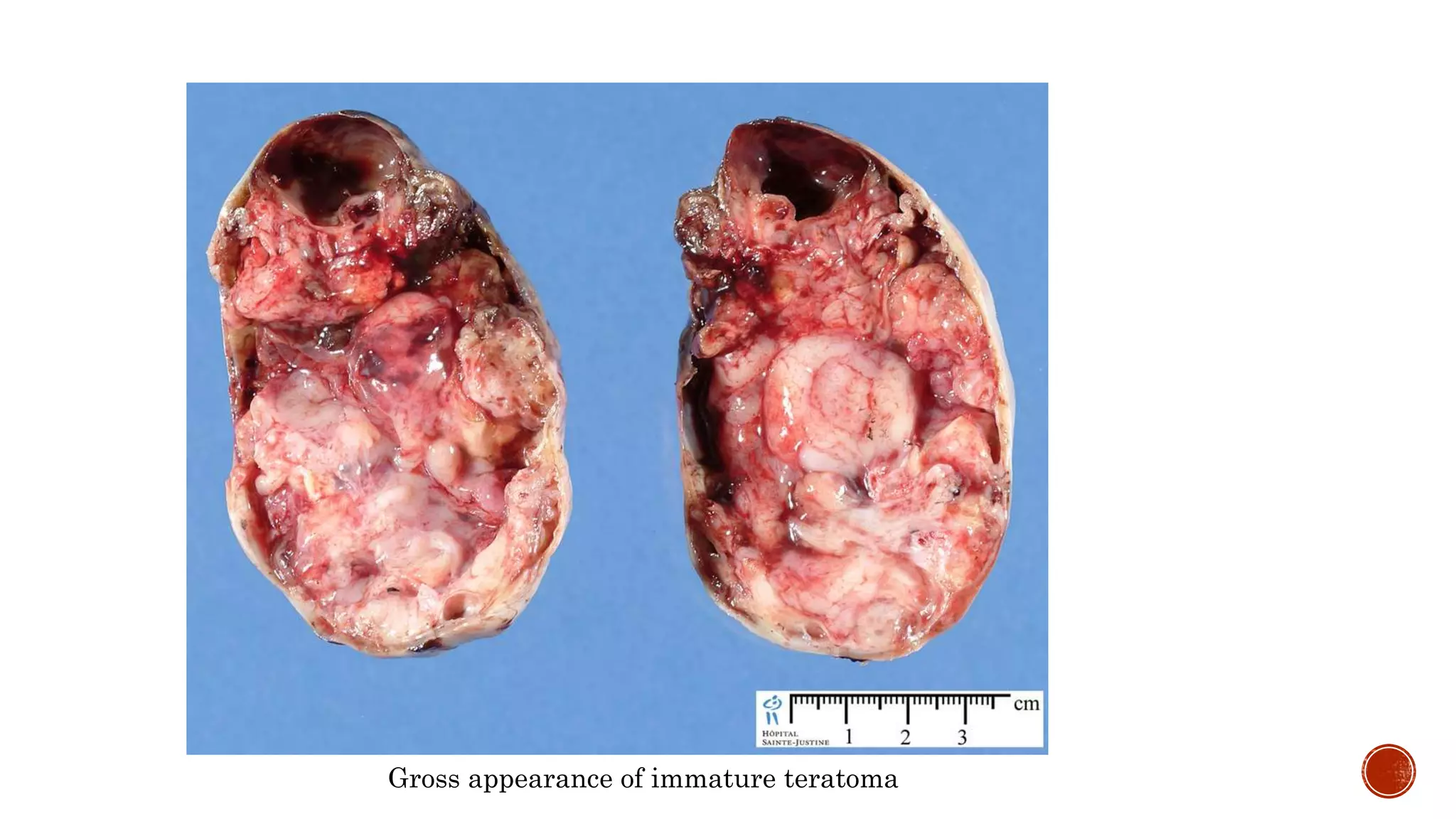
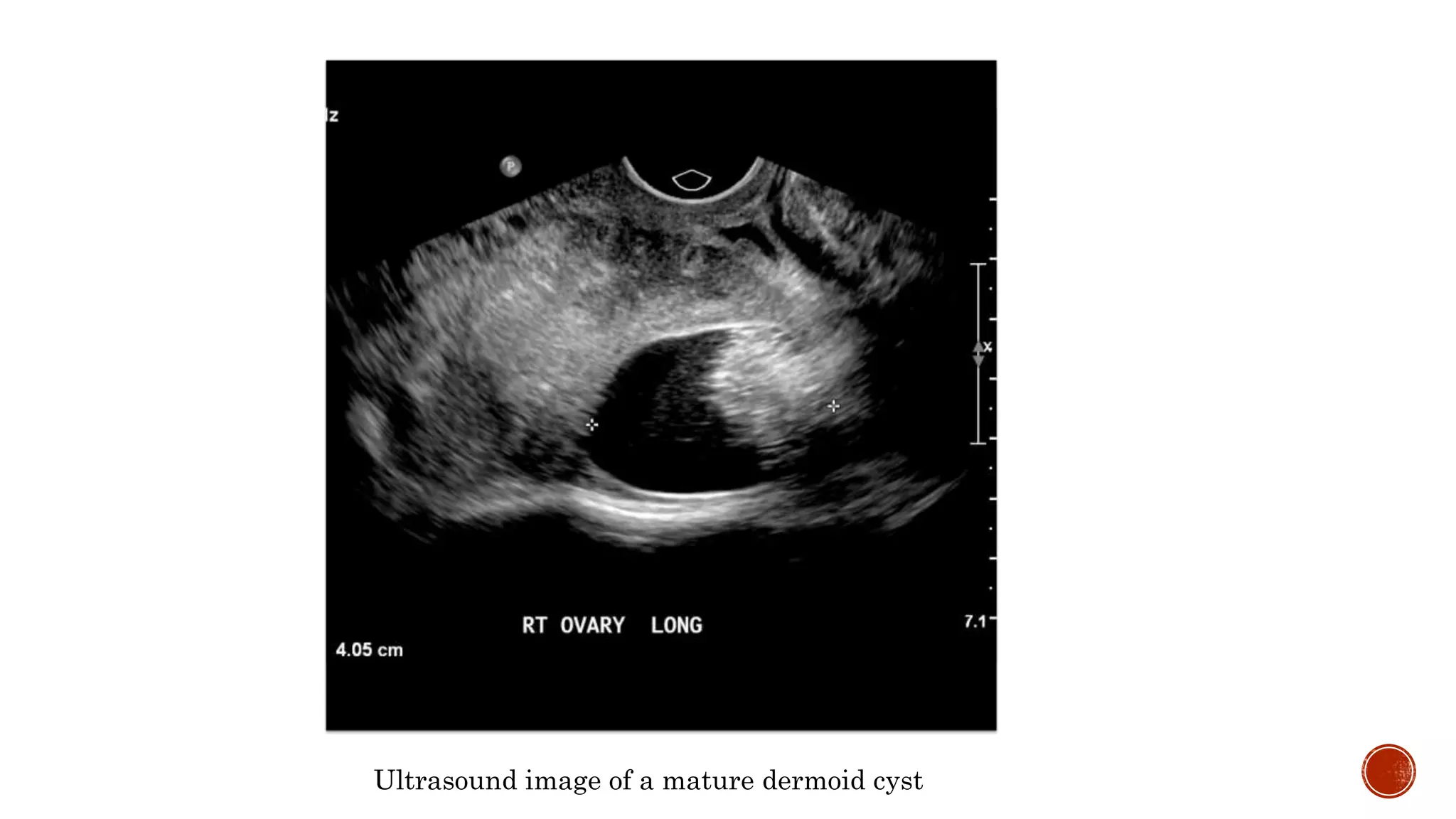
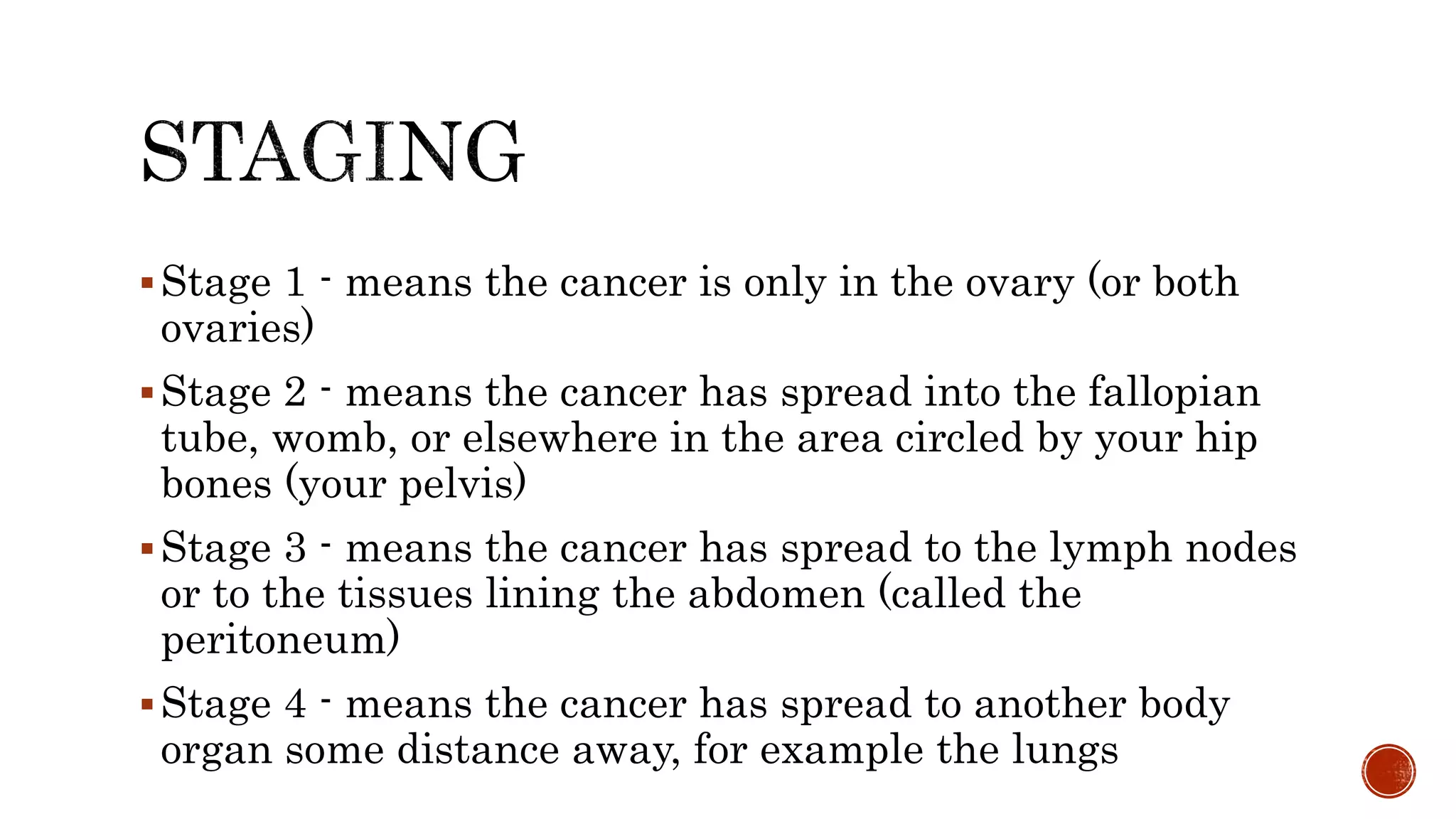
This document discusses teratomas, which are embryonic tumors containing tissues from all three germ layers. It describes the different types of teratomas including mature cystic, immature, and monodermal. Mature cystic teratomas are most common and typically benign. Immature teratomas have a small risk of malignancy. Complications can include torsion, rupture, or malignant transformation. Diagnosis involves imaging and lab tests. Treatment is surgical excision with chemotherapy sometimes needed for immature types. Recurrence risks depend on maturity and completeness of resection.