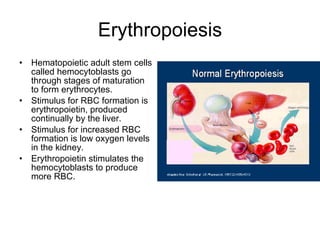
Blood homeostasis depends on the continual transport of components to and from cells. The composition of blood includes plasma, which makes up 55% of blood, and formed elements such as red blood cells, white blood cells, and platelets, which make up the remaining 45%. Blood disorders can involve abnormalities in any of the formed elements, including anemias that decrease oxygen-carrying capacity, leukocyte disorders like leukemia, and clotting disorders such as hemophilia or thrombosis.