This document provides information about different types of bites including frost bites, human bites, and animal bites. It summarizes the key points about each type of bite as follows:
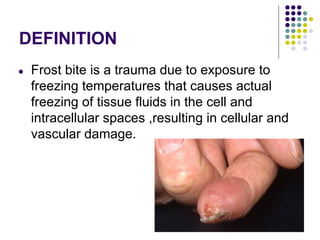
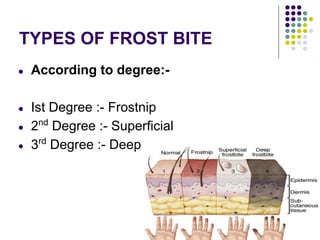
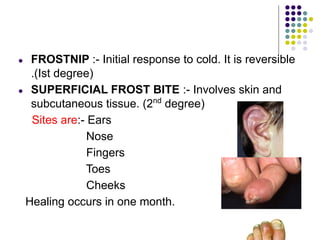
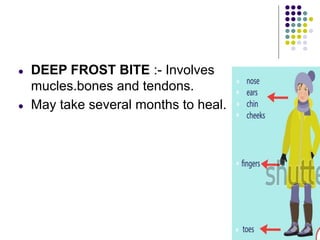
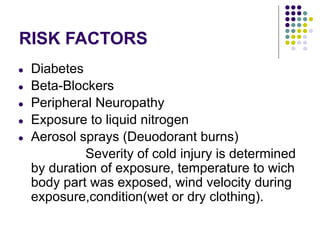
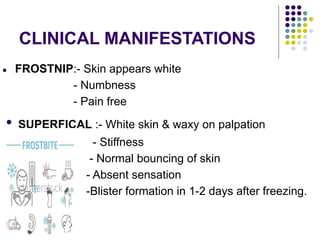
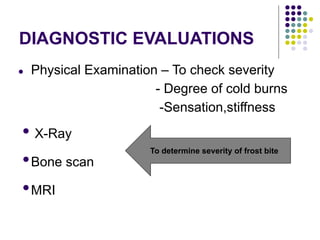
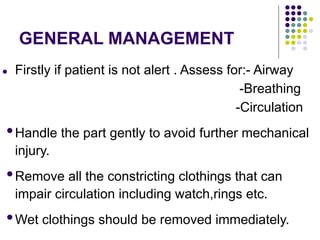
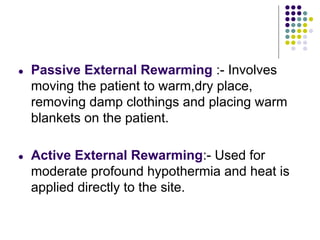
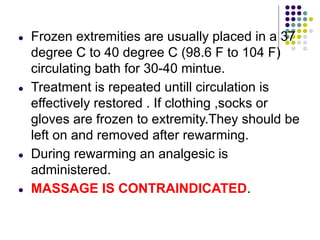
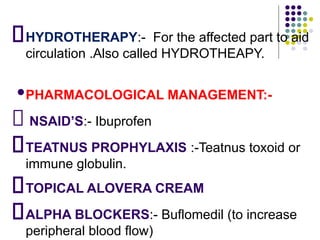
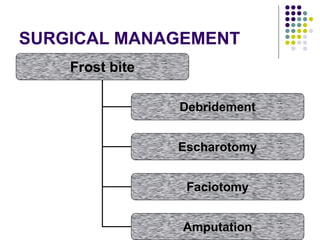
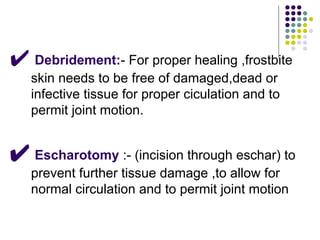
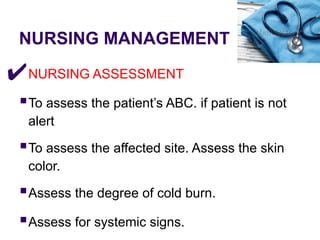
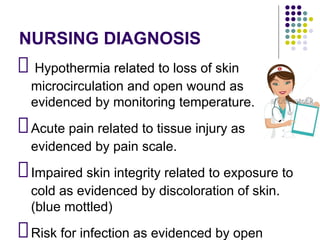
Frost bites are caused by freezing of tissues due to exposure to cold temperatures and wind. They can range from superficial to deep tissue damage. Signs include numbness, blistering, and loss of sensation. Treatment focuses on slowly rewarming tissues.
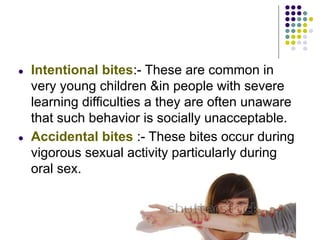
Human bites often occur during fights and among young males using alcohol. They carry risk of infection. Wounds should be cleaned and raised, with prompt medical care.
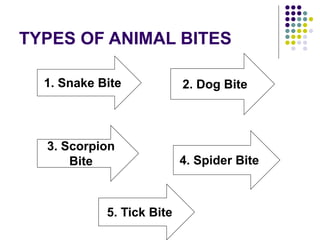
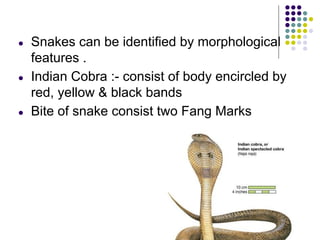
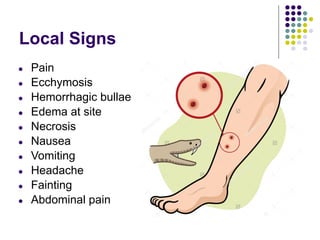
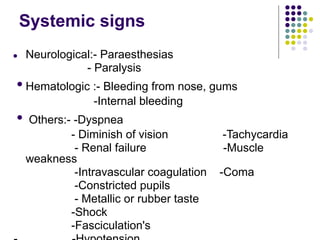
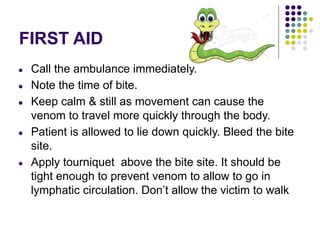
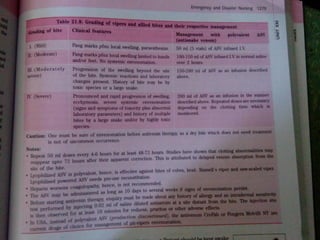
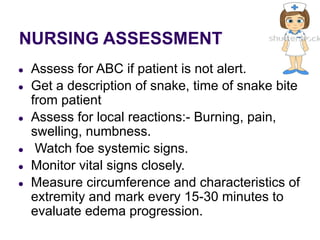
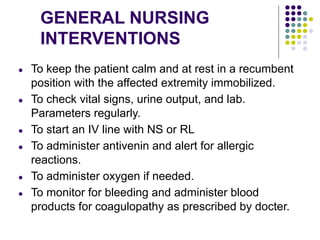
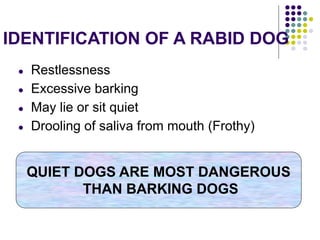
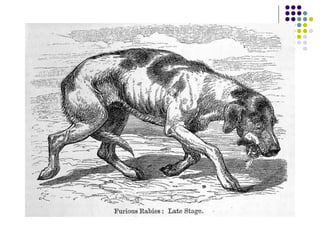
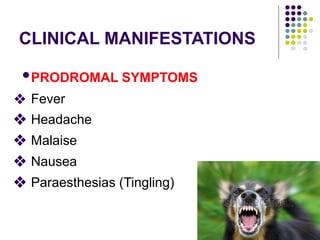
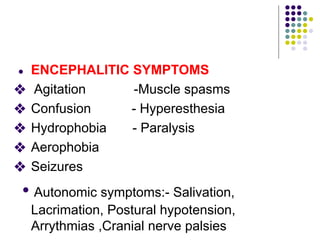
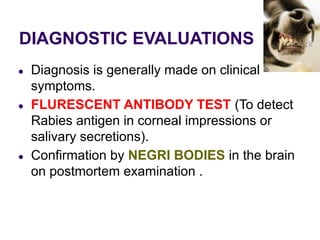
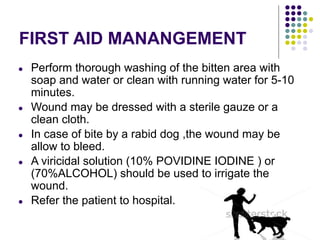
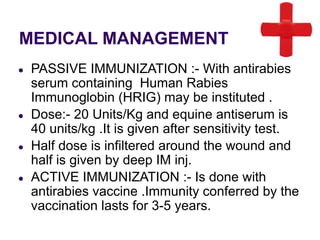
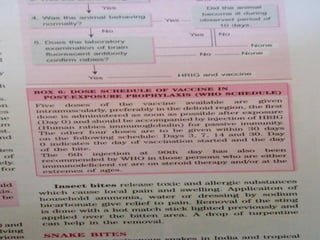
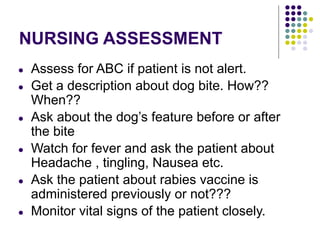
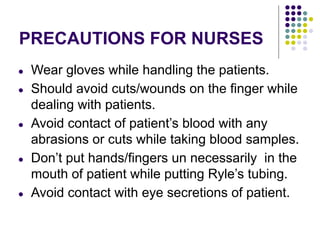
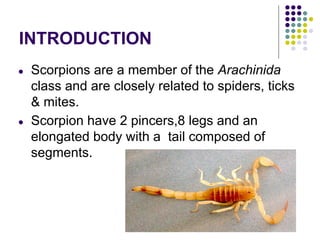
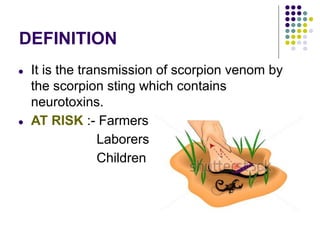
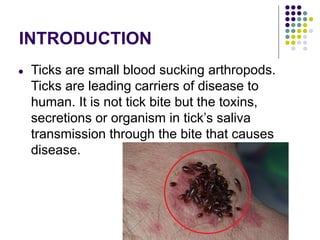
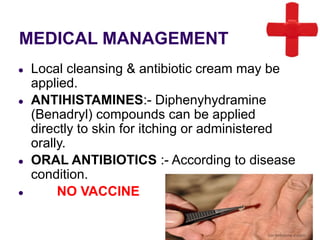
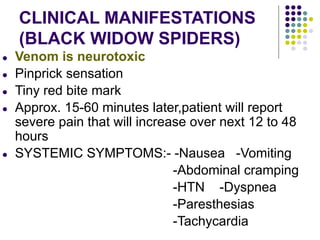
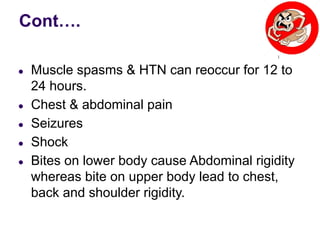
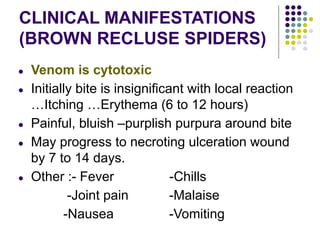
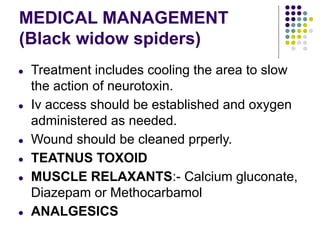
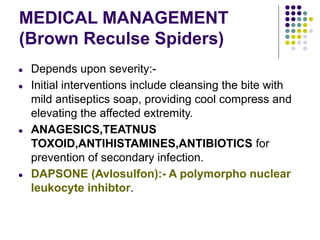
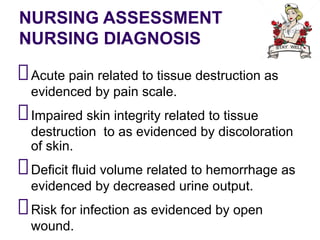
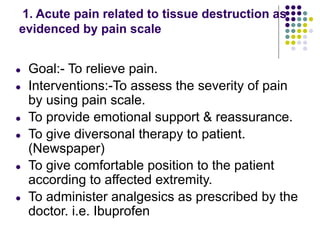
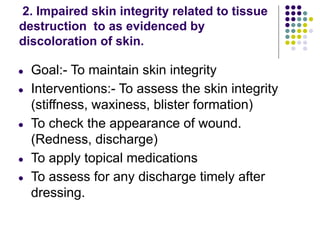
Animal bites mainly come from snakes, dogs, and spiders. Snake bites can cause local or systemic poisoning. Signs