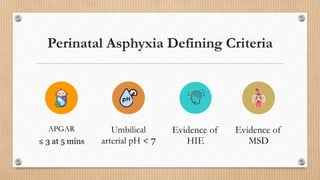
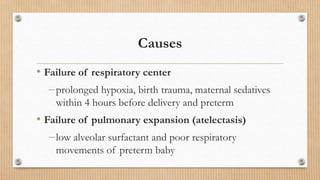
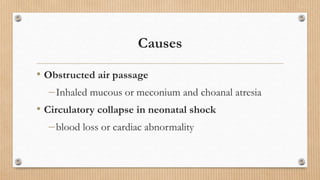
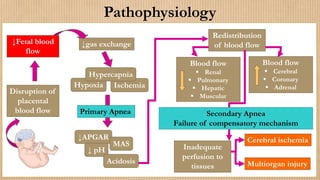
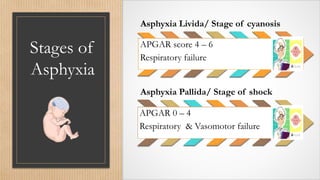
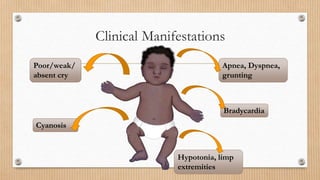
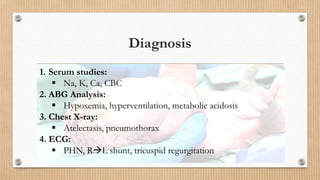
1) Asphyxia neonatorum, or perinatal asphyxia, is the failure to establish spontaneous respiration immediately after birth, which can be caused by factors that lead to hypoxia such as respiratory failure, airway obstruction, or circulatory collapse.
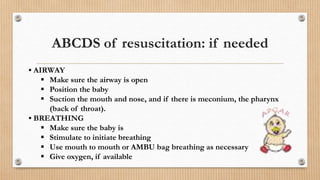
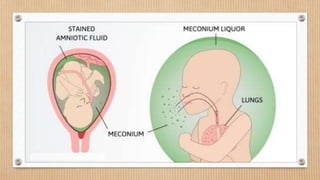
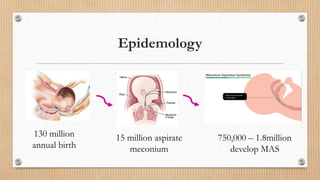
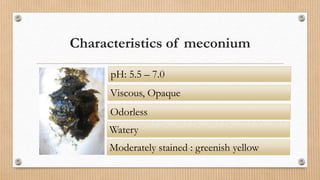
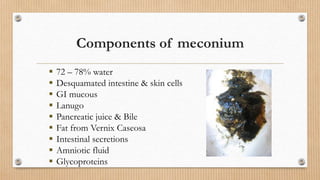
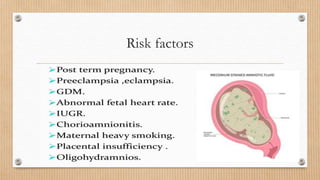
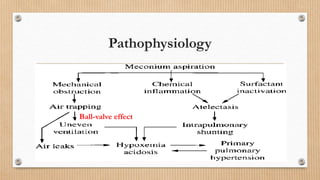
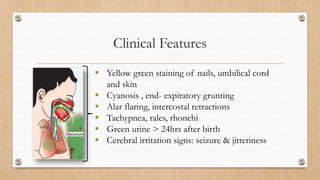
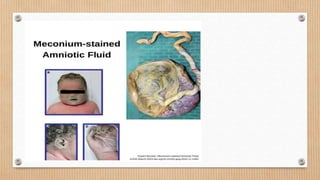
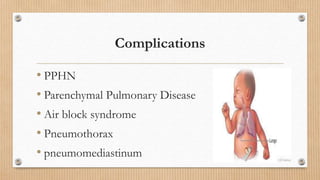
2) Meconium aspiration syndrome is a respiratory condition caused by aspiration of meconium, the newborn's first stool, into the lungs before or during delivery, which can cause inflammation and obstruction of the airways.
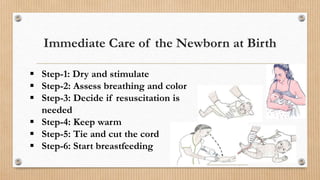
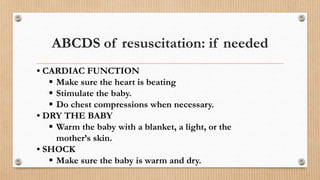
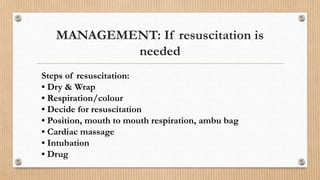
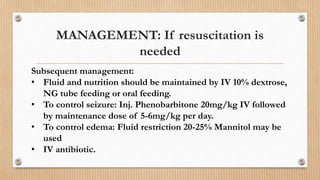
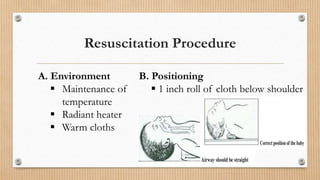
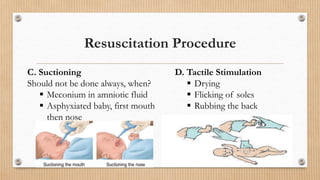
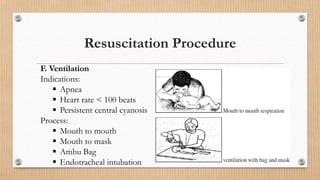
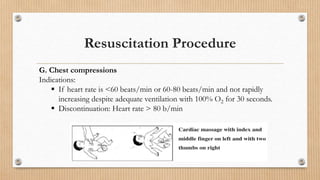
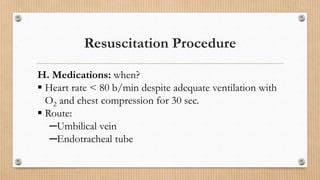
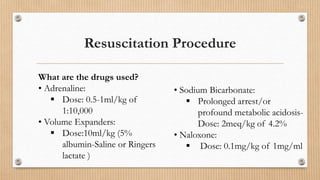
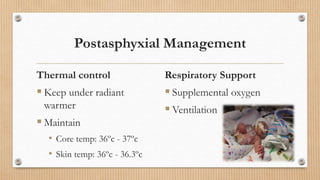
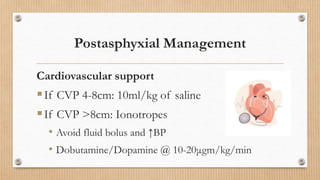
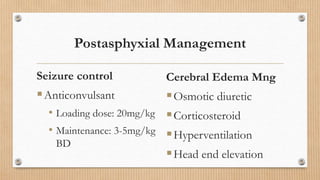
3) Treatment for both conditions involves resuscitation and stabilization of the newborn, including clearing the airways, stimulating breathing, warming the infant, and providing respiratory and circulatory support as needed. Ongoing