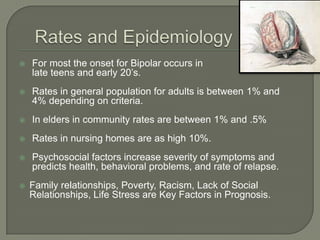
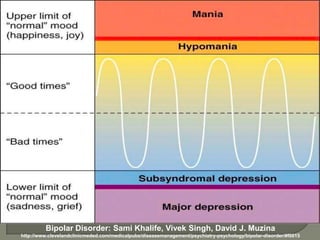
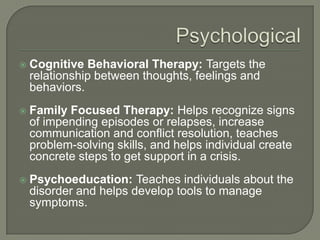
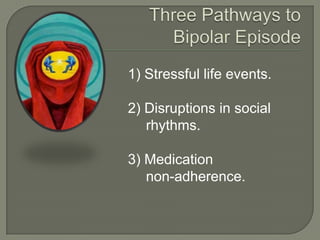
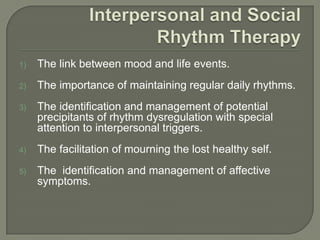
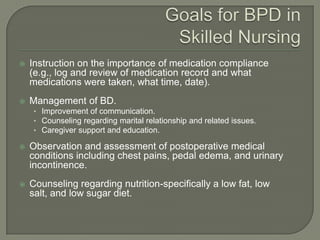
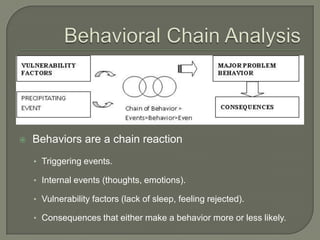
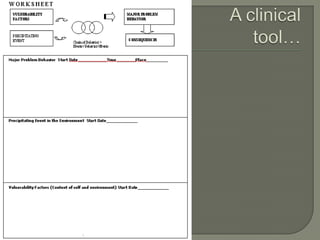
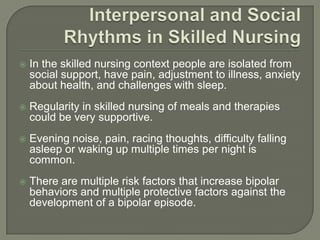
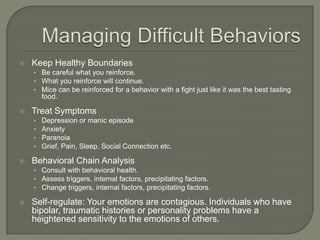
The document discusses mood and behavior management for patients with bipolar disorder in skilled nursing facilities. It notes that those in skilled nursing often face isolation, health issues, and sleep disturbances that can trigger bipolar episodes. Effective management includes maintaining regular routines, treating underlying symptoms, using behavioral chain analysis to address triggers, and helping staff regulate their own emotions to avoid exacerbating patients' conditions.