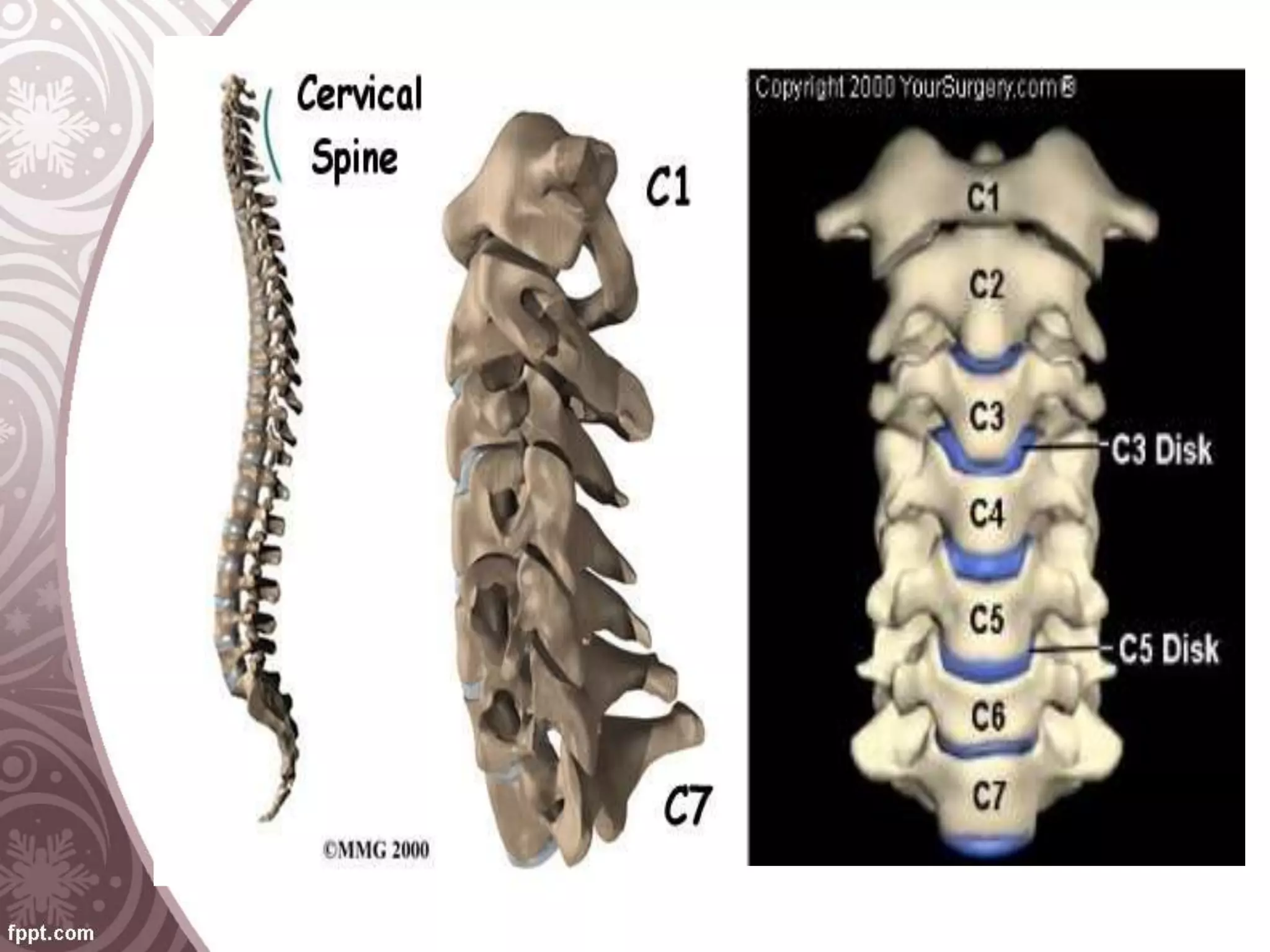
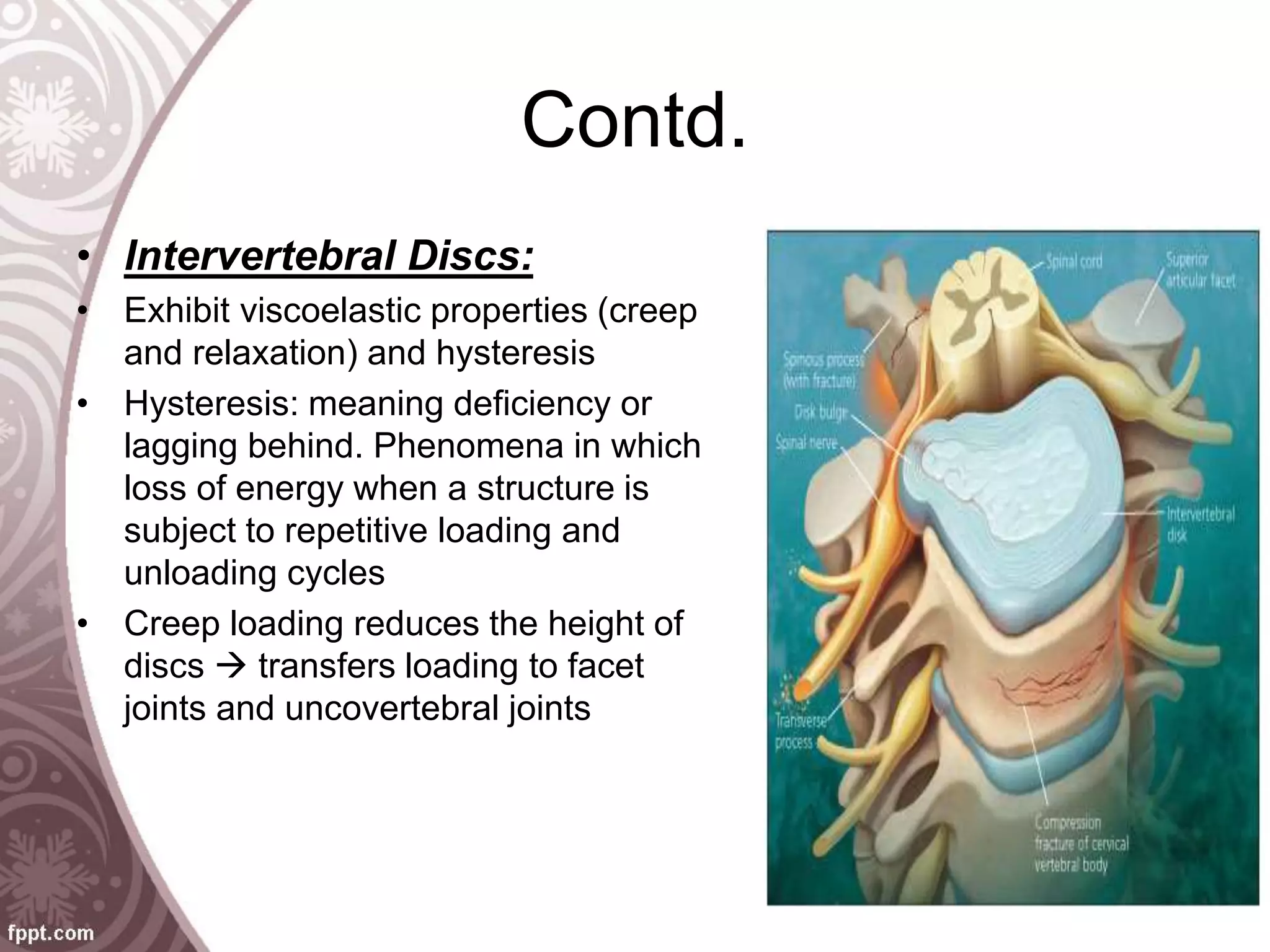
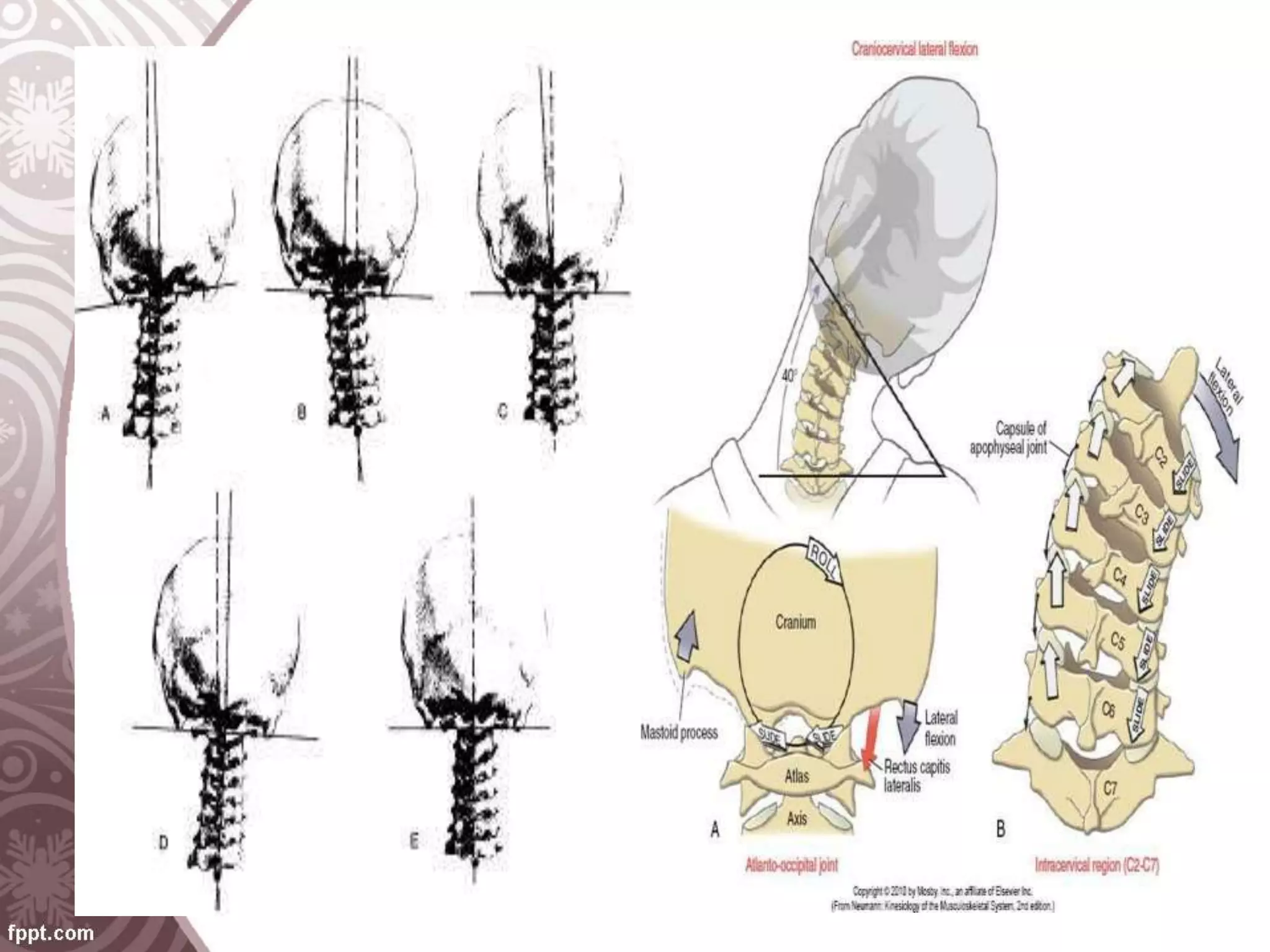
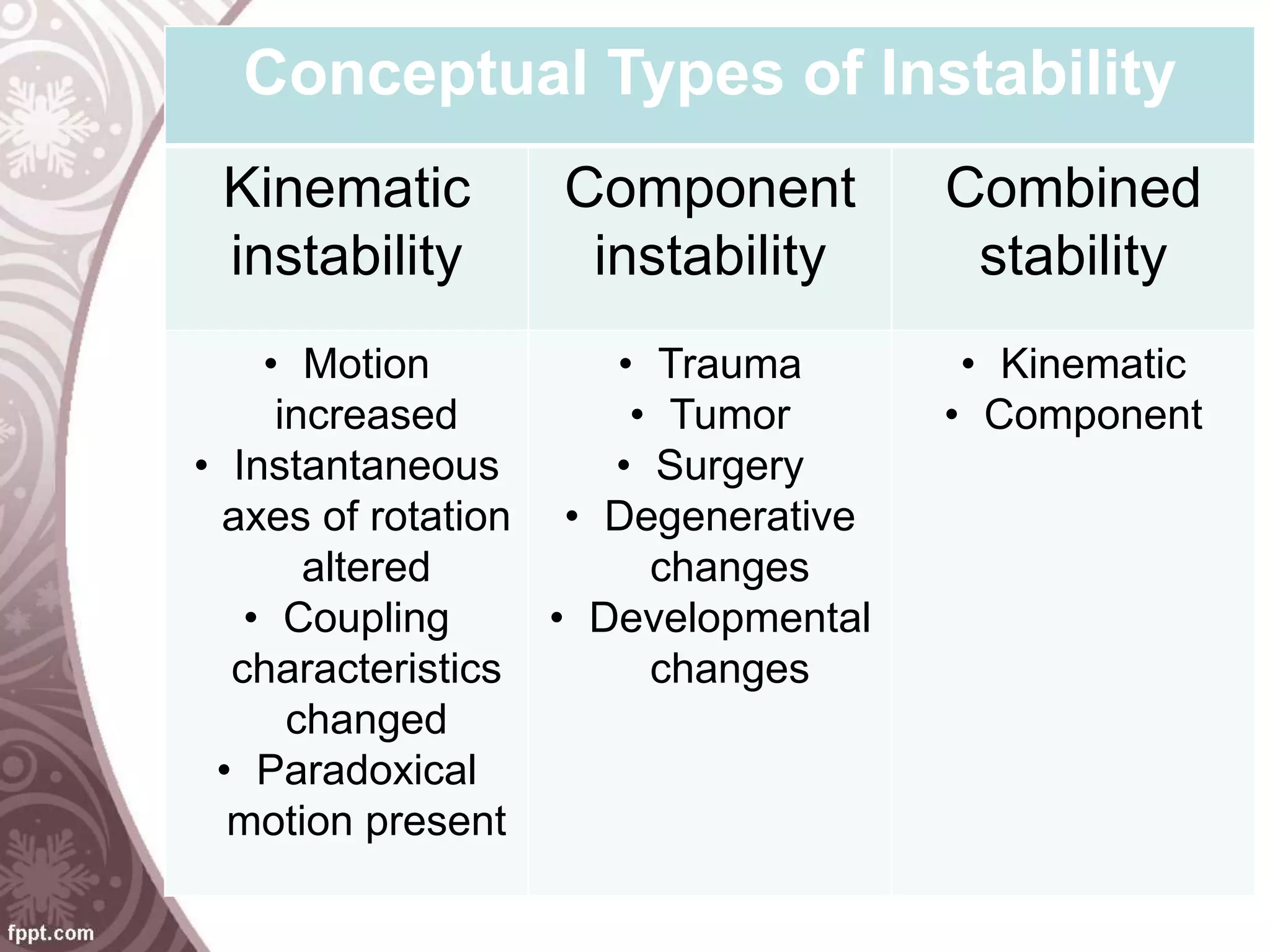
The document discusses the biomechanics of the cervical spine. It covers the anatomy of bony structures and intervertebral discs, as well as the mechanical properties of vertebrae, discs, ligaments, muscles and neural elements. It describes the importance of kinematics including range of motion, surface joint motion, and spinal stability. It also discusses biomechanics concepts such as decompression, arthrodesis, cervical spine fixation, and cervical trauma from injuries like whiplash.