MRI Workshop
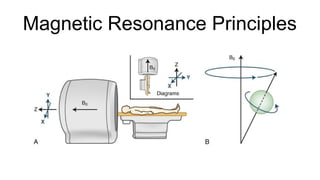
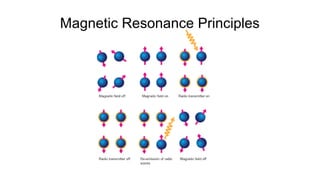
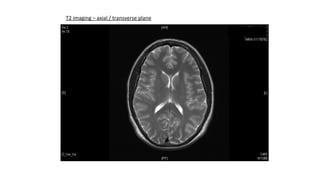
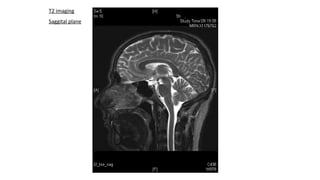
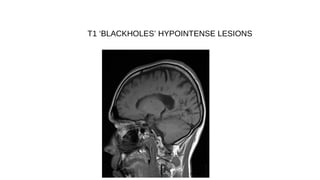
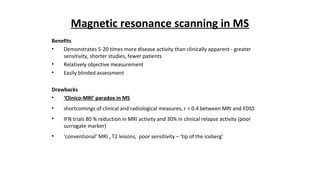
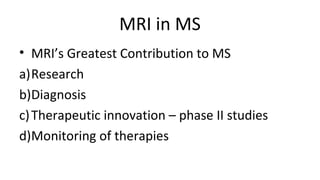
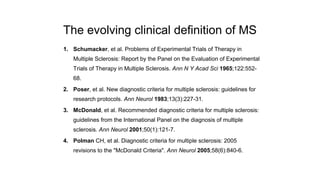
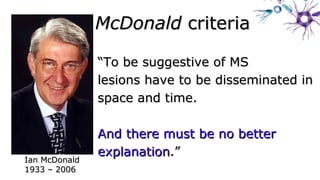
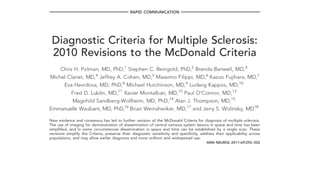
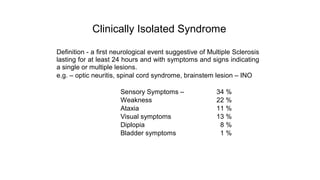
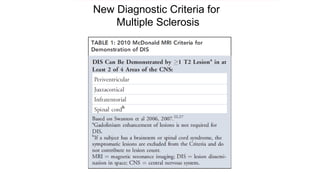
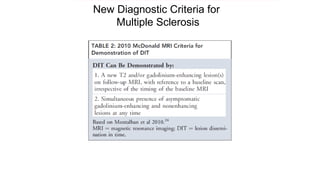
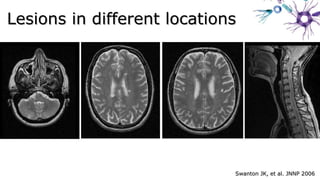
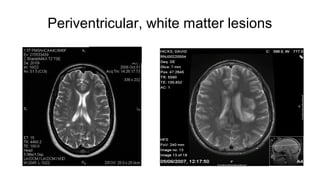
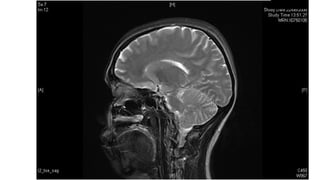
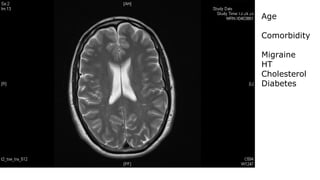
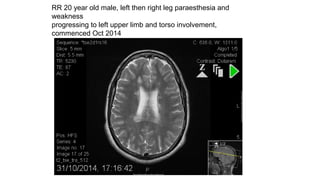
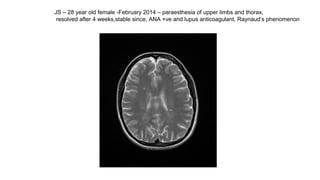
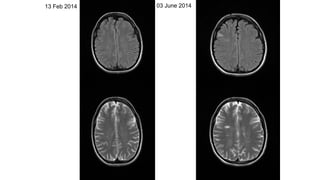
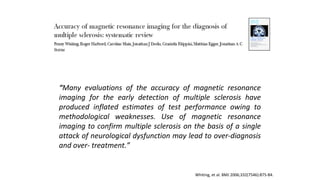
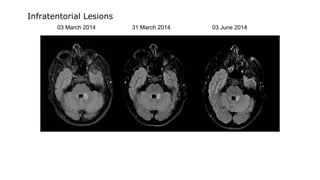
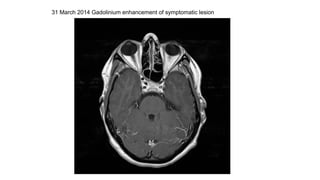
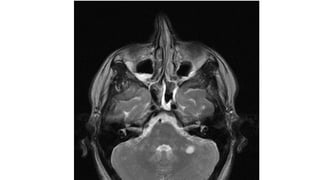
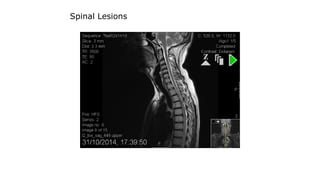
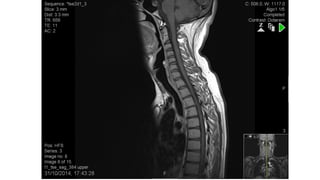
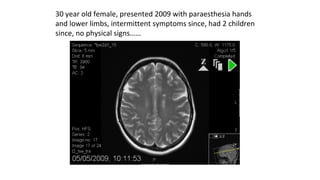
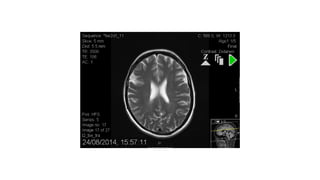
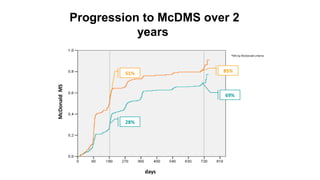
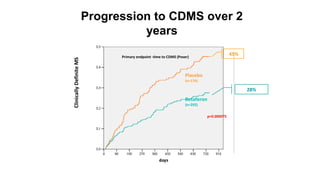
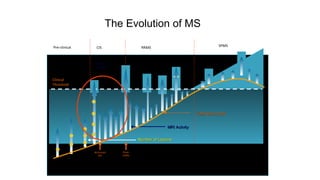
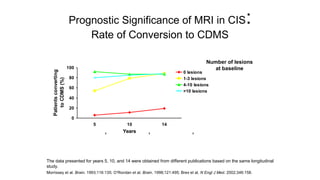
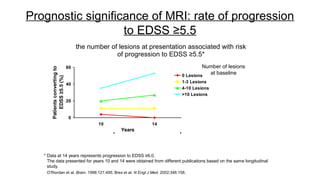
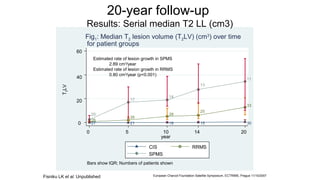
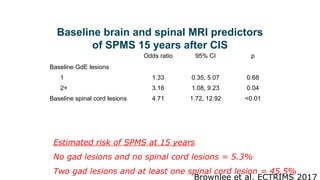
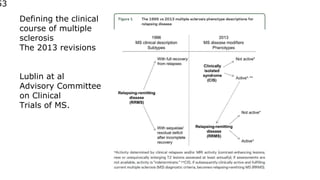
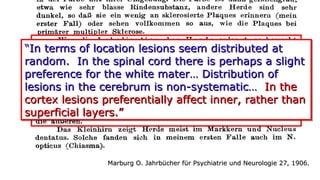
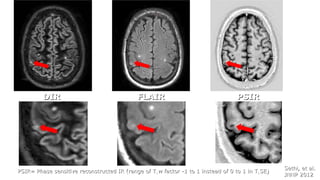
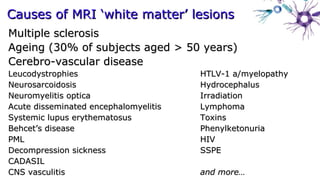
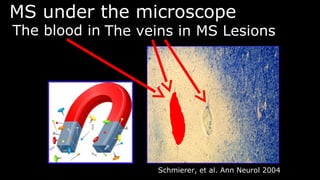
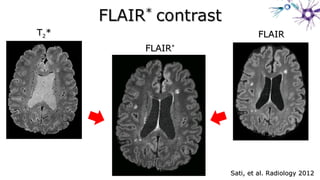
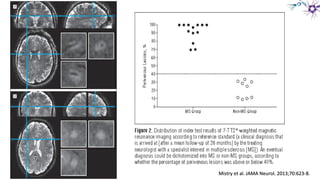
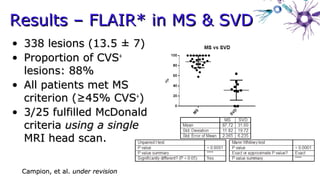
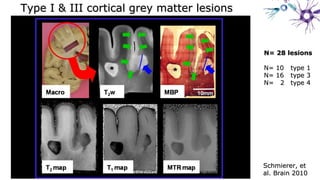
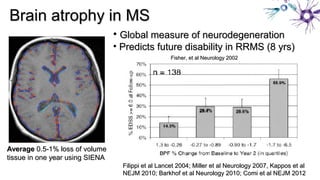
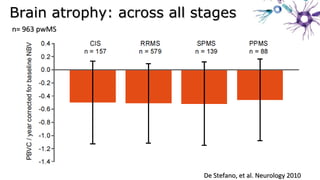
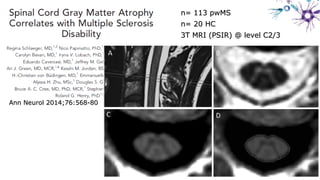
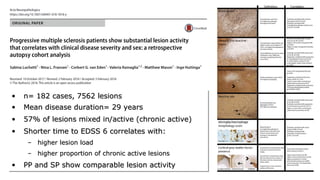
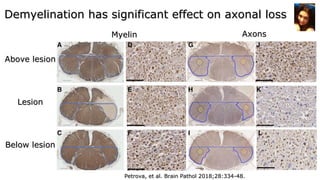
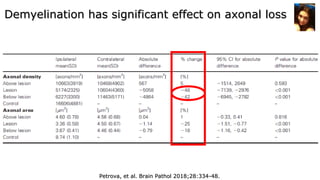
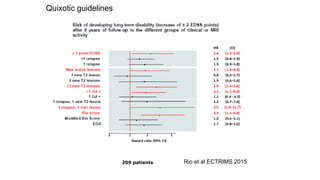
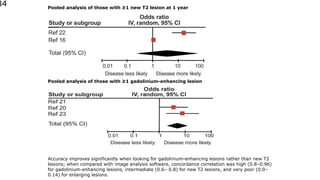
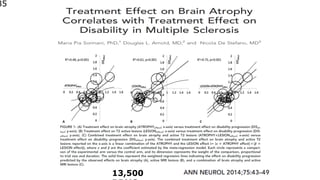
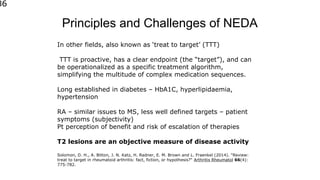
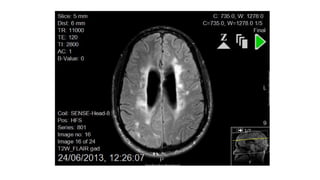
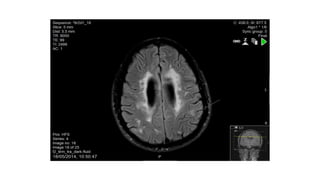
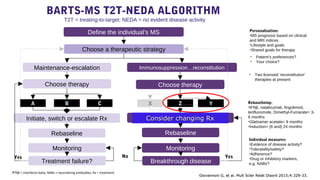
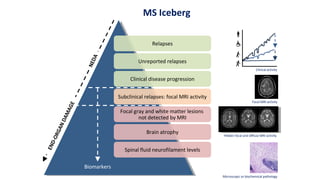
Dr. Ben Turner held an MRI workshop in November 2018. He discussed the principles of magnetic resonance imaging, different MRI techniques like T2 imaging and flair images, and how MRI is beneficial but also has drawbacks for monitoring multiple sclerosis. MRI is most useful for research, diagnosis, therapeutic innovation for drug trials, and monitoring therapies. New diagnostic criteria for multiple sclerosis were also presented, focusing on dissemination of lesions in space and time with no better explanation. Factors like lesion number and location provide prognostic information about progression.