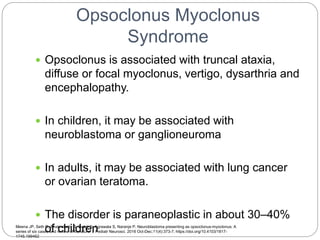
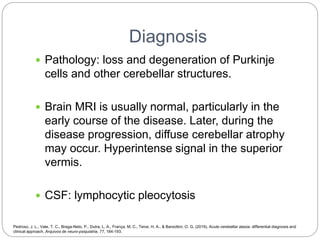
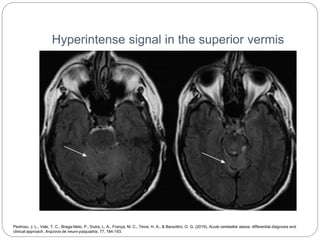
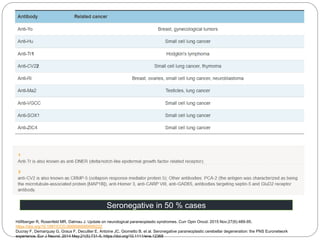
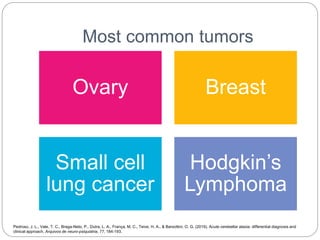
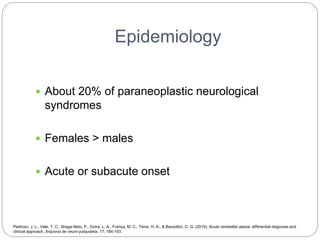
This document discusses paraneoplastic ataxia, which occurs in about 20% of paraneoplastic neurological syndromes. The most common primary tumors associated with paraneoplastic ataxia are ovarian, breast, small cell lung cancer, and Hodgkin's lymphoma. Clinical manifestations include acute or subacute onset of gait ataxia, truncal ataxia, limb ataxia, dysarthria, and nystagmus. Diagnosis involves looking for loss of Purkinje cells on pathology, MRI showing possible cerebellar atrophy or hyperintense signal in the superior vermis, and lymphocytic pleocytosis on CSF. Treatment involves surgically resecting the primary tumor if possible
![Clinical Manifestation
Acute or subacute onset of vertigo, dizziness,
vomiting, and nausea, and evolves rapidly, over
weeks to months, to gait ataxia, truncal and limb
ataxia, dysarthria and nystagmus
Other signs and symptoms may be present,
including dysphagia, brisk reflexes, hearing loss,
extrapyramidal signs, peripheral neuropathy and
cognitive impairment
Kuwabara S. [Pathophysiology of ataxia in Fisher syndrome]. Brain Nerve. 2016 Dec;68(12):1411-4. Japanese. https://doi.org/10.11477/mf.1416200610
Vernino S. Paraneoplastic cerebellar degeneration. Handb Clin Neurol. 2012;103:215-23. https://doi.org/10.1016/B978-0-444-51892-7.00013-9
Leypoldt F, Wandinger KP. Paraneoplastic neurological syndromes. Clin Exp Immunol. 2014 Mar;175(3):336-48. https://doi.org/10.1111/cei.12185](https://image.slidesharecdn.com/paraneoplasticataxia-220311050353/85/Paraneoplastic-Ataxia-5-320.jpg)