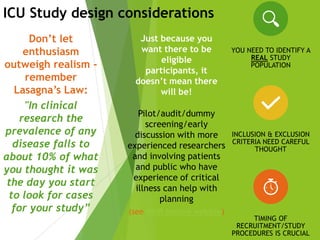
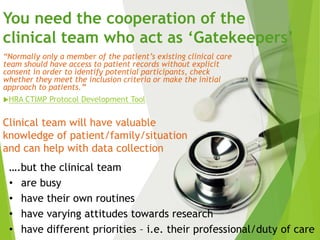
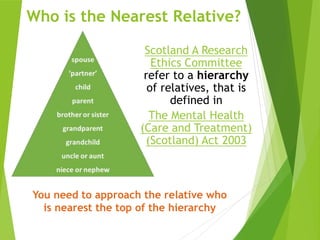
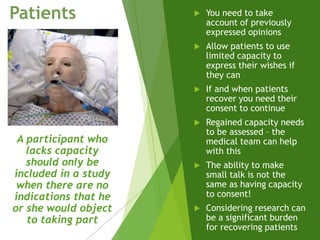
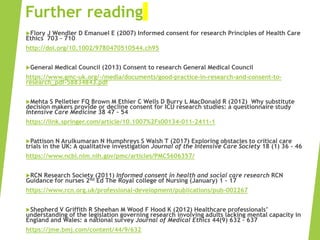
This document serves as a beginner’s guide to conducting ICU research in Edinburgh, covering challenges, study design, and patient consent. It emphasizes the importance of cooperation with clinical teams and the ethical considerations when dealing with patients who lack the capacity to consent. Key topics include identifying suitable research populations, approaching family members for consent, and ensuring compliance with Scottish laws governing research ethics.