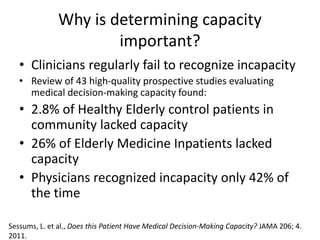
The document discusses the critical aspects of assessing medical decision-making capacity, highlighting the prevalence of incapacity among elderly patients and the role of clinicians in recognizing this issue. It outlines the specific and dynamic nature of medical capacity, requirements for evaluation, and the importance of surrogate decision-makers. Additionally, it provides tools for capacity assessment and emphasizes that patients with decision-making capacity have the right to refuse treatments.