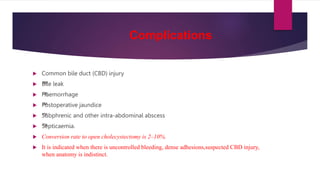
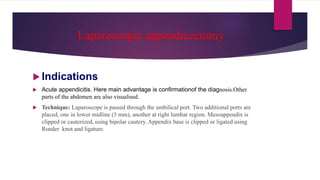
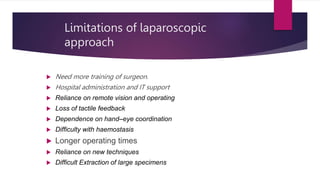
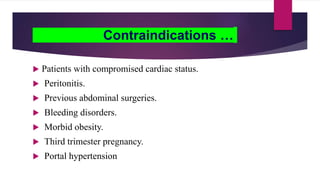
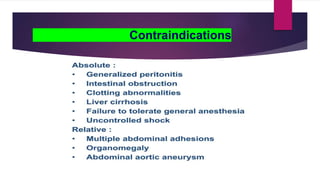
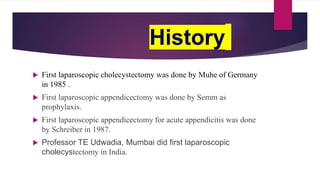
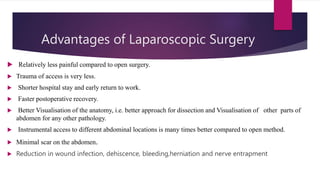
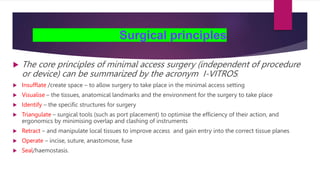
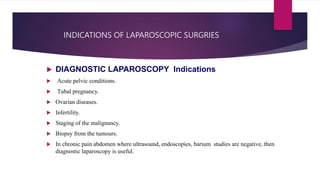
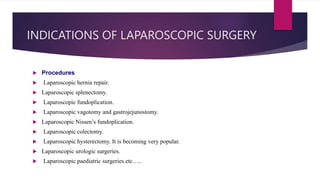
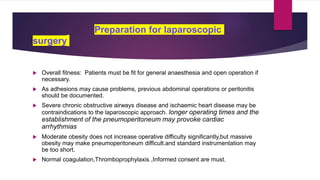
This document discusses the basics of laparoscopic surgery, including its history, advantages, surgical principles, and various types of laparoscopic procedures like cholecystectomy and appendectomy. It emphasizes the reduced recovery time, minimized pain, and improved visualization compared to open surgery. Additionally, it covers preparation, instruments, complications, and contraindications associated with laparoscopic surgeries.

![Instruments Used
Zero degree and 30°
laparoscope is
commonly used. Side
viewing scopes [30°]
have better
visualisation .](https://image.slidesharecdn.com/basicsoflaproscopicsurgery-230402172730-2d0fd3c7/85/Basics-of-laparoscopic-surgery-pptx-18-320.jpg)