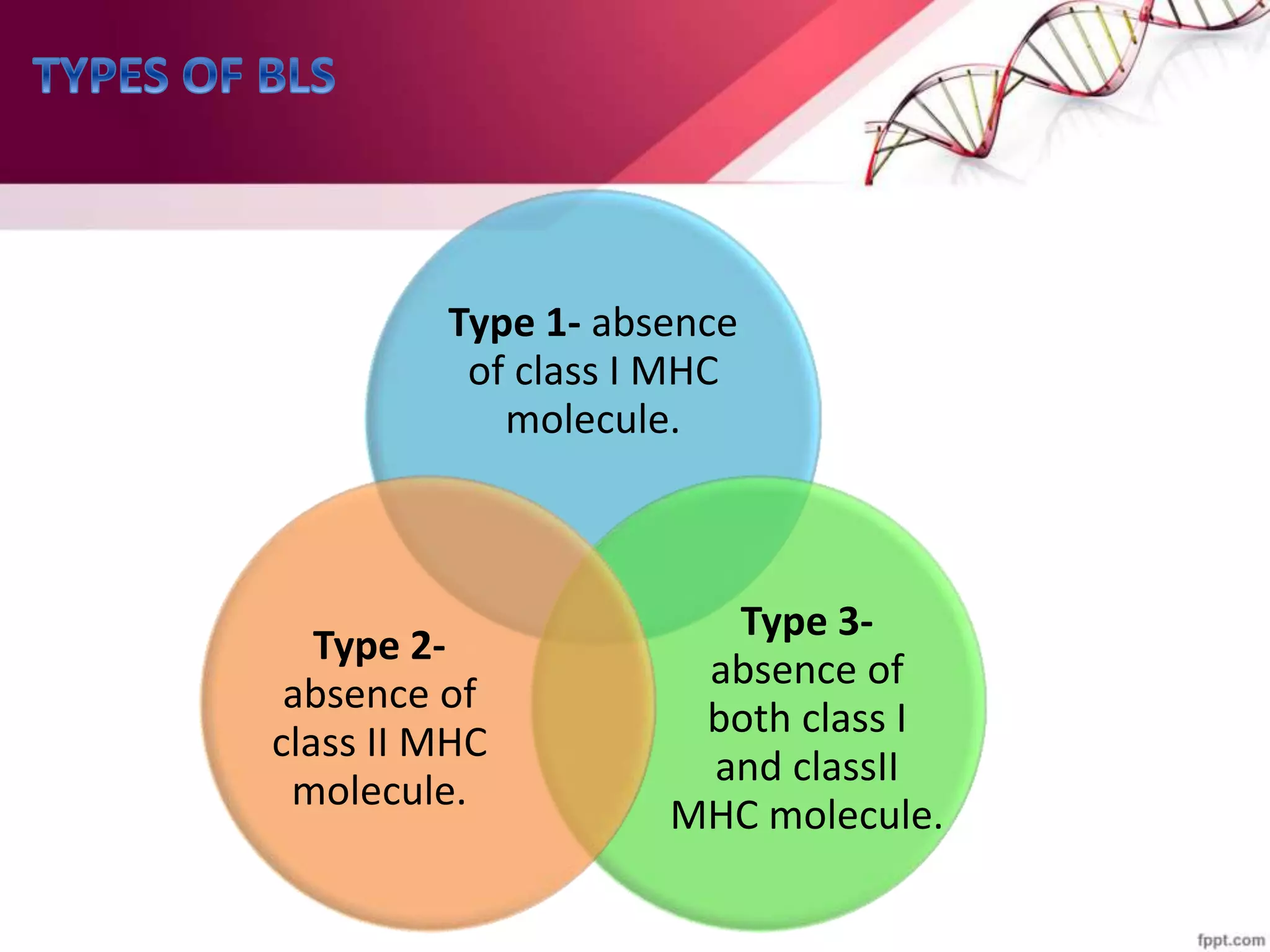
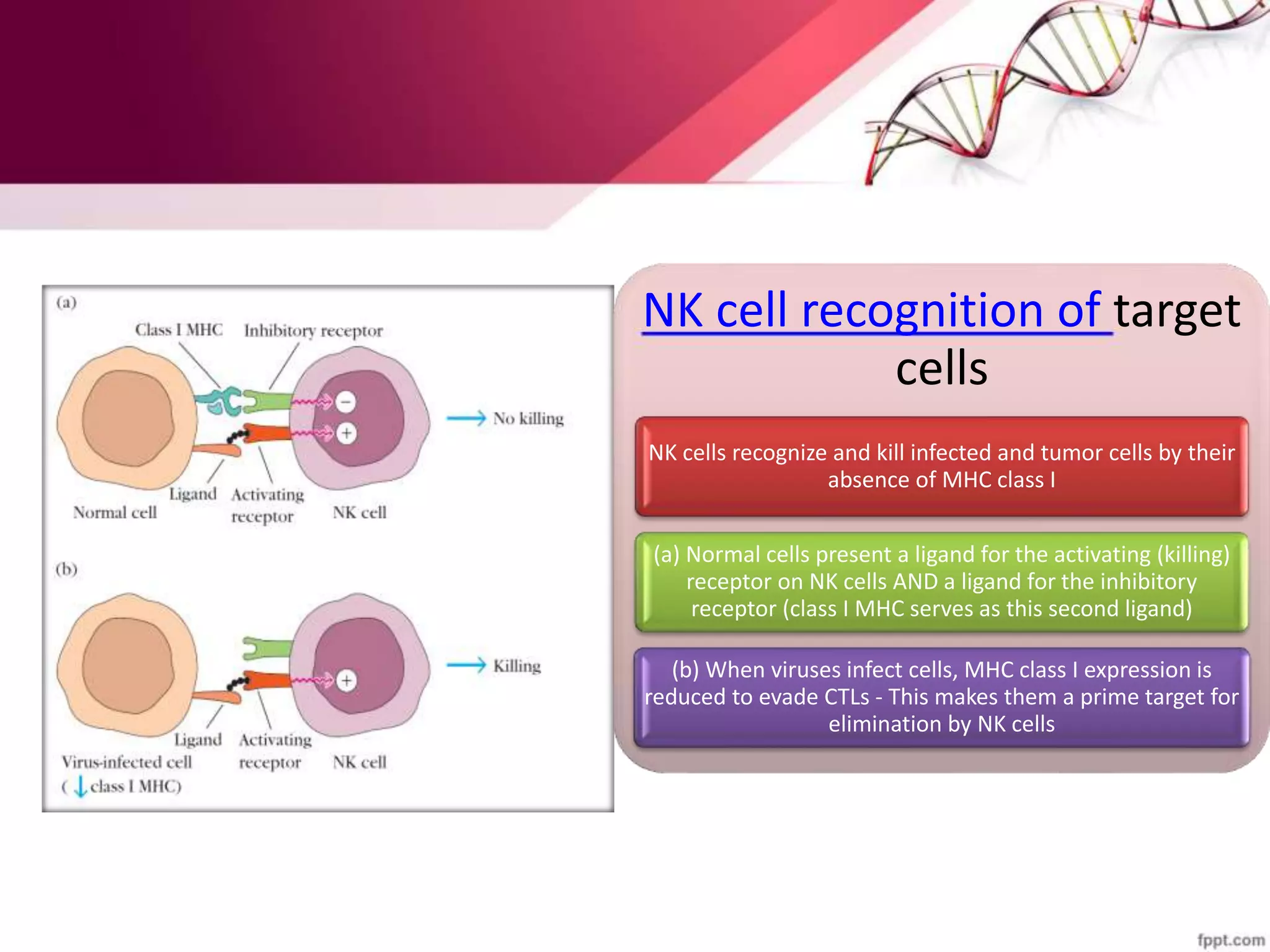
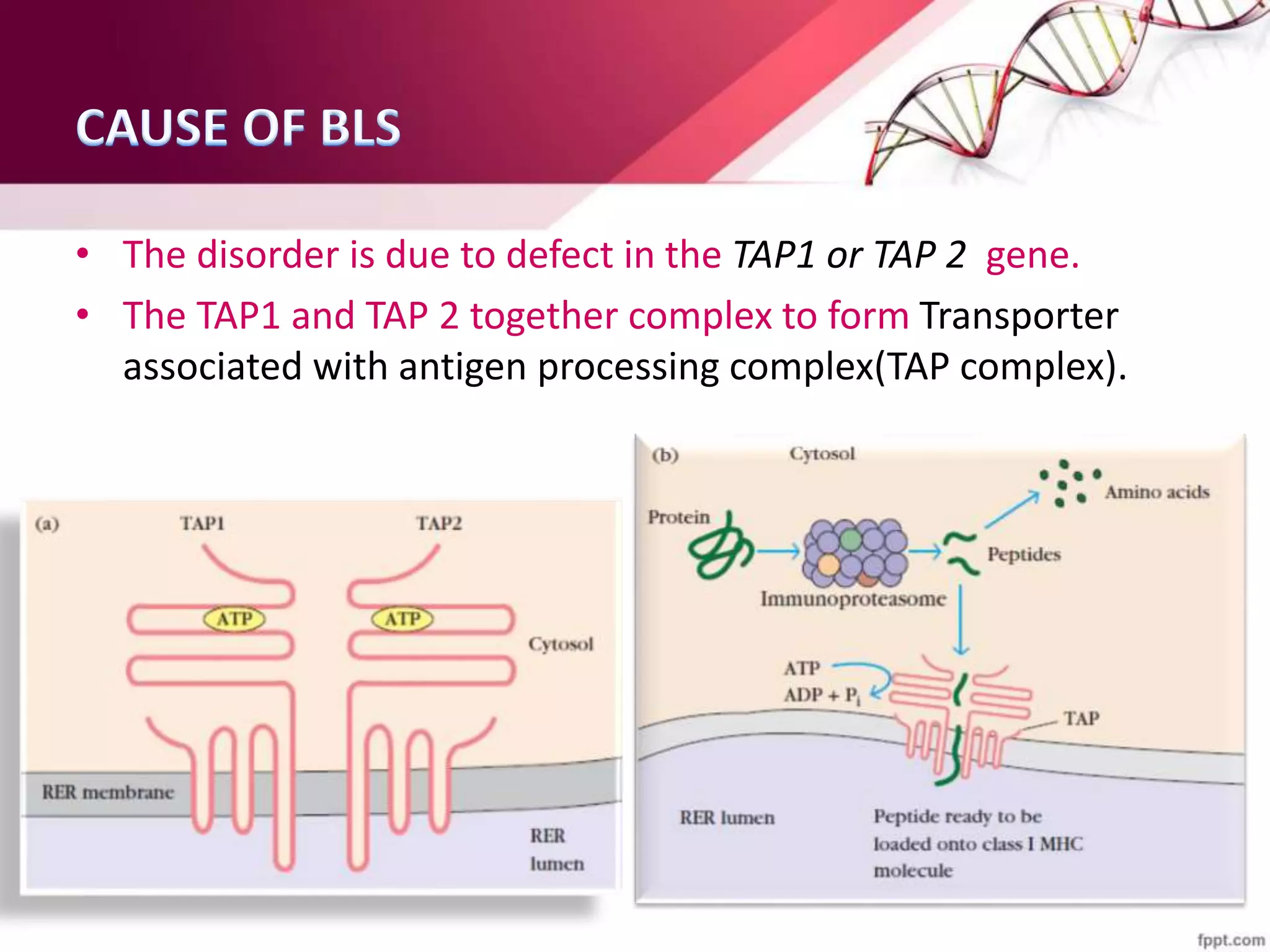
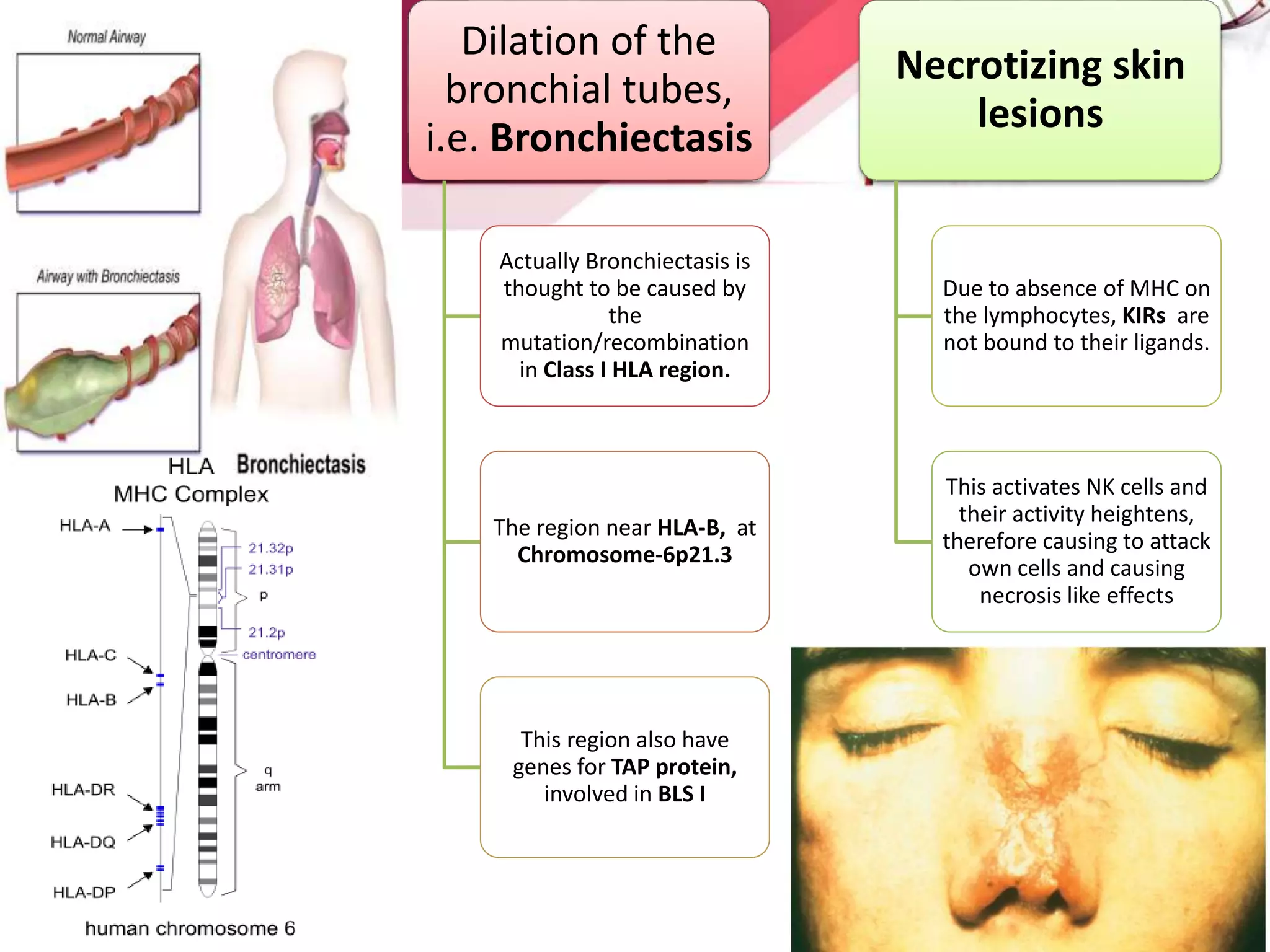
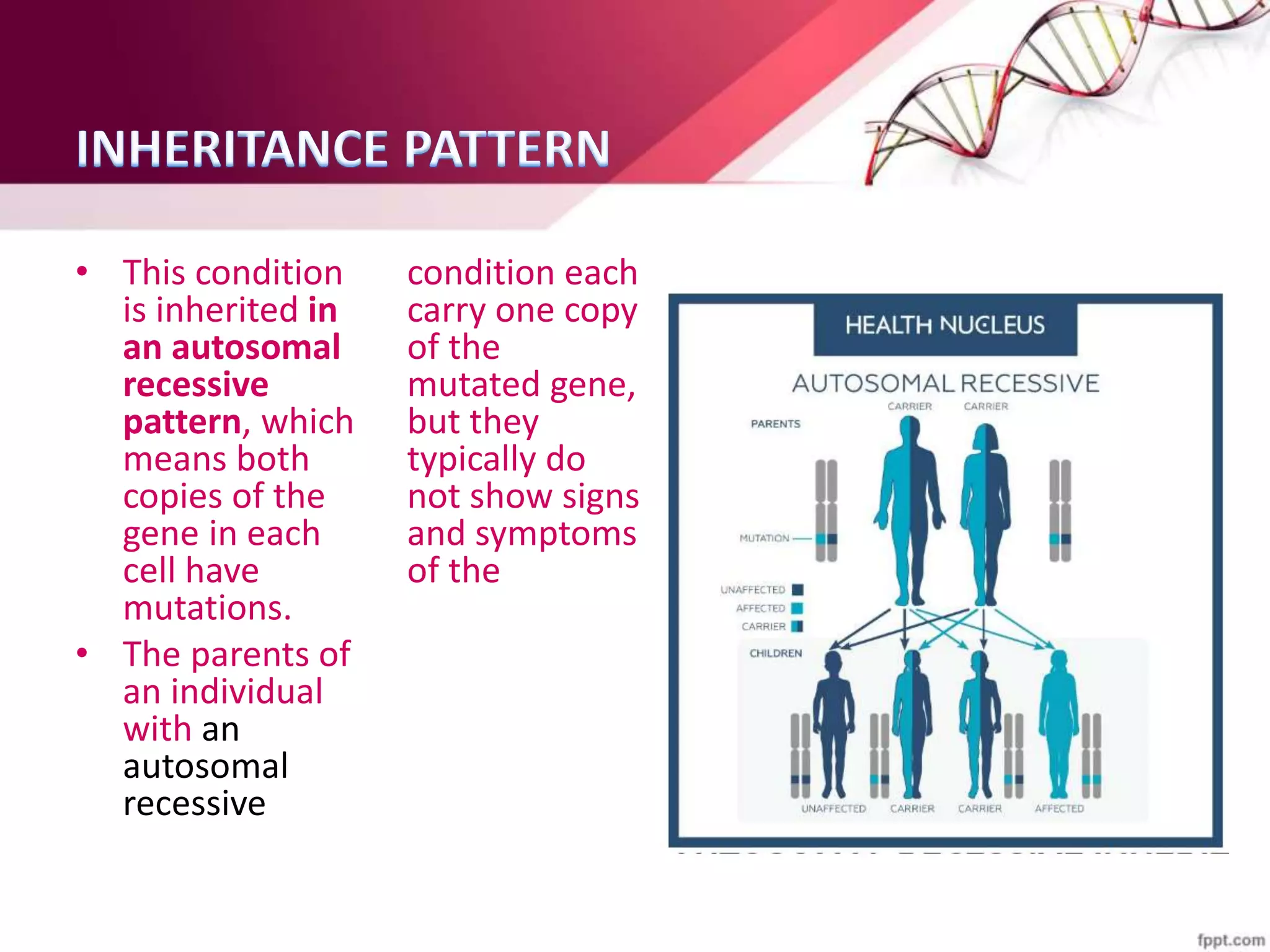
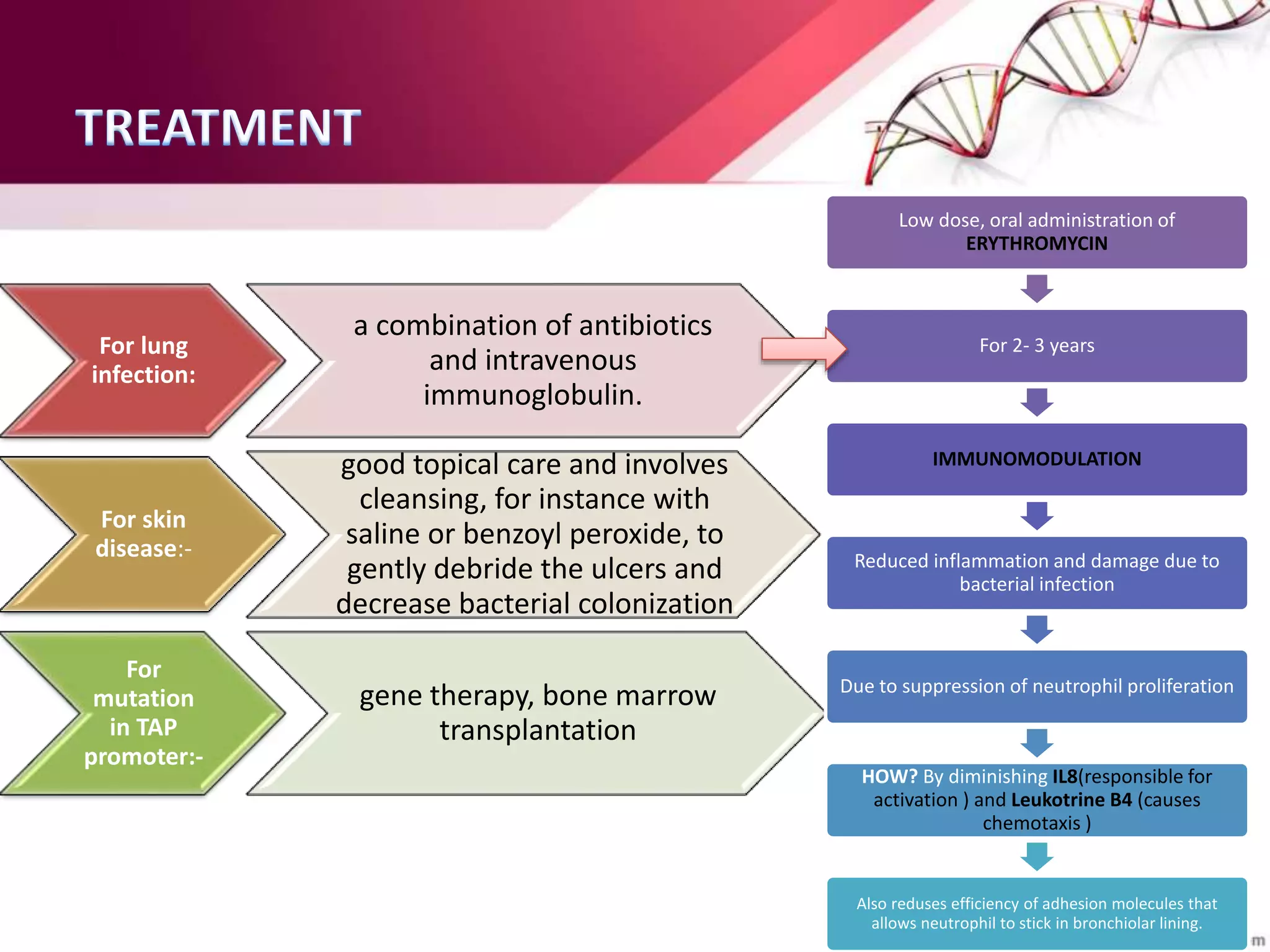
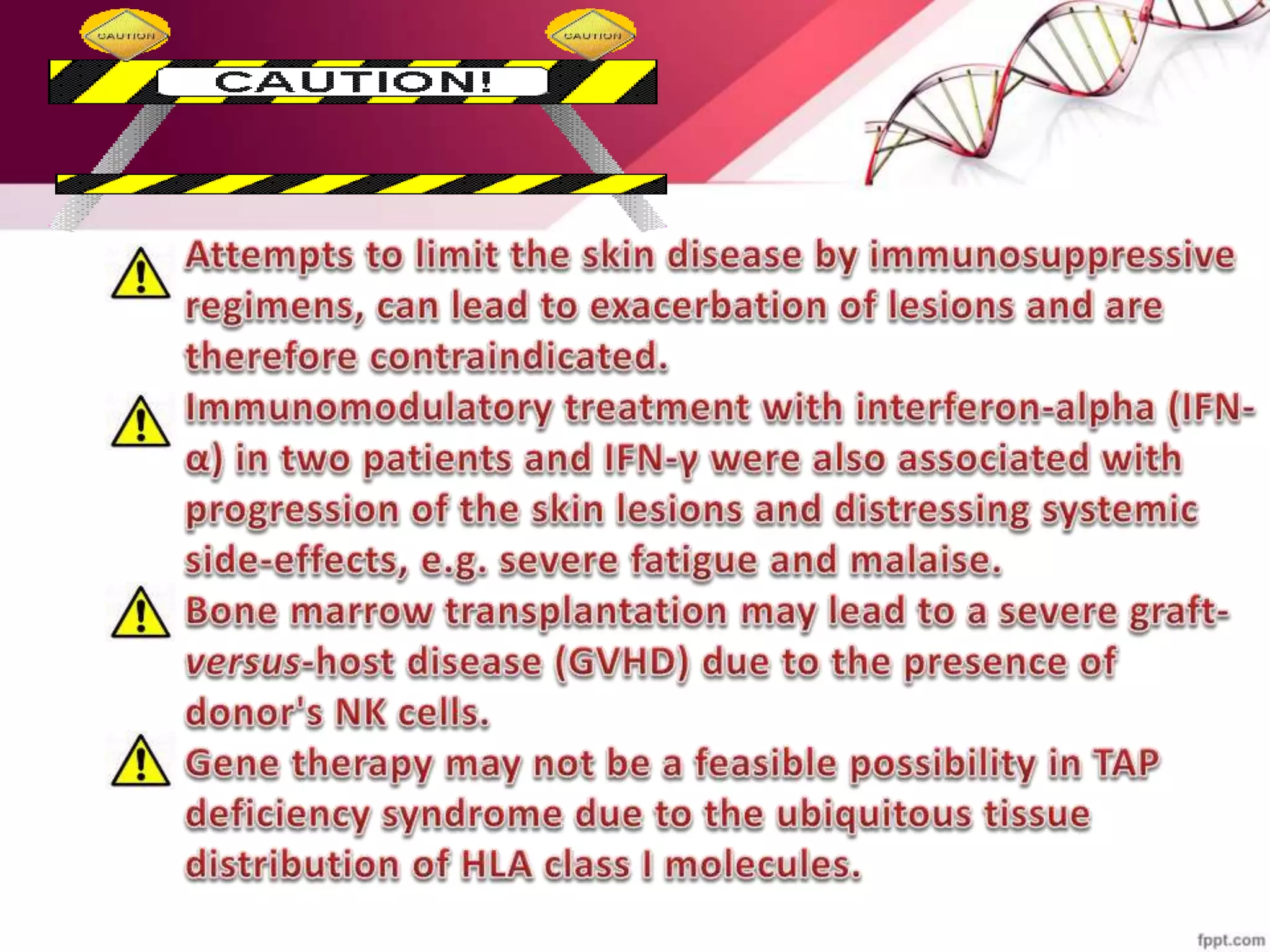
BLS (Bare Lymphocyte Syndrome) is a rare genetic immuno-deficiency disorder characterized by the absence of MHC or HLA on lymphocytes, leading to a fragile immune system similar to SCID. It is caused by mutations in genes related to MHC class I and II molecules, resulting in cellular abnormalities such as increased NK and γδ T cells while decreasing CD8+ αβ T cells. The condition is inherited in an autosomal recessive pattern and can lead to severe infections, requiring treatments like antibiotics, immunoglobulin, and potentially gene therapy or bone marrow transplantation.