This document discusses bacterial toxins, including endotoxins and exotoxins. It provides details on:
- Endotoxins are lipopolysaccharides found in the outer membrane of gram-negative bacteria. They are released when bacteria die and can cause systemic inflammation.
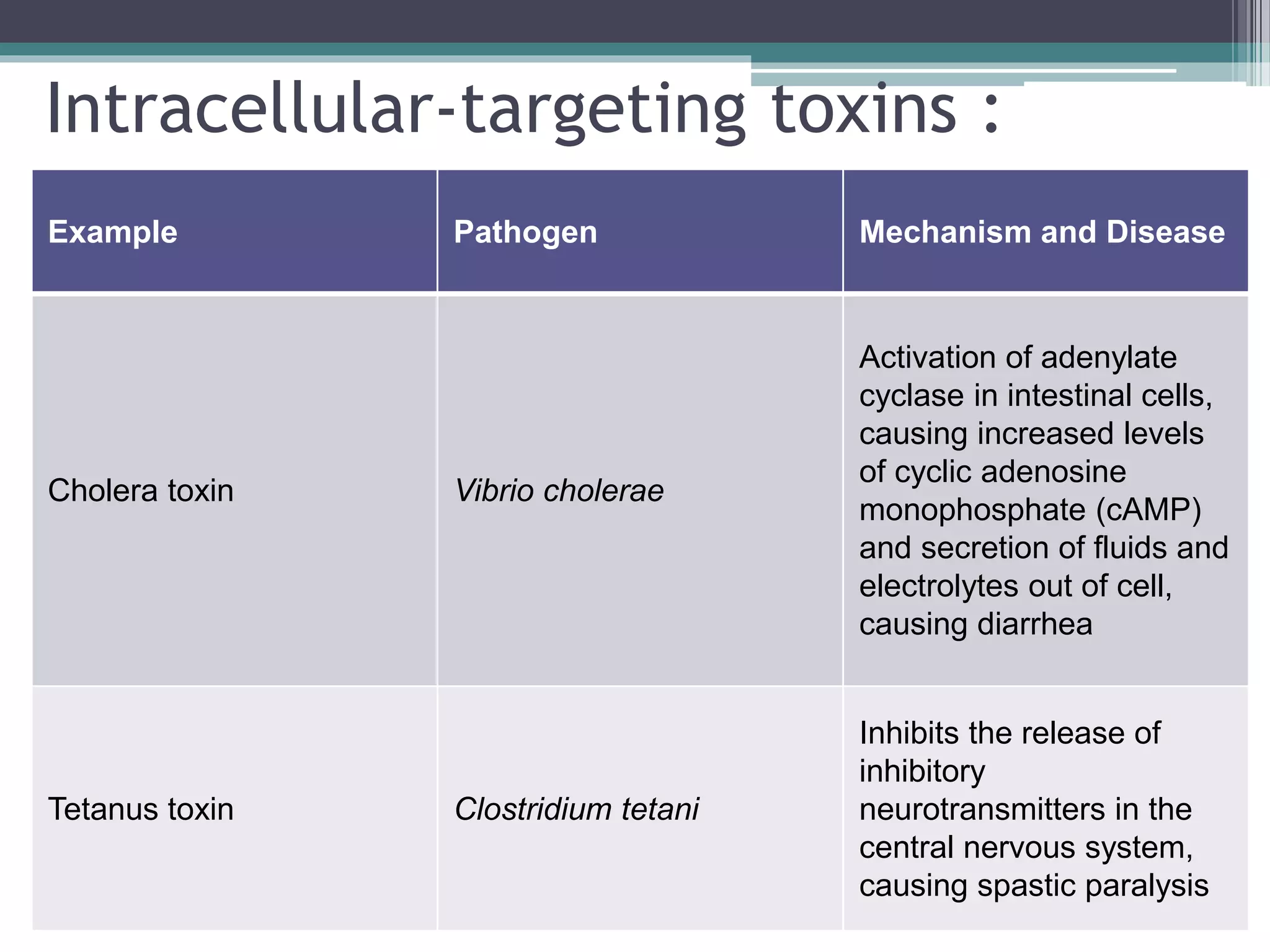
- Exotoxins are protein toxins produced by both gram-positive and gram-negative bacteria that have specific targets and mechanisms of action. Examples include cholera toxin, tetanus toxin, and diphtheria toxin.
- Bacterial toxins can cause diseases like cholera, typhoid fever, and hepatitis by damaging host cells and tissues or disabling the immune system. The liver, kidneys, sweat, and digestive