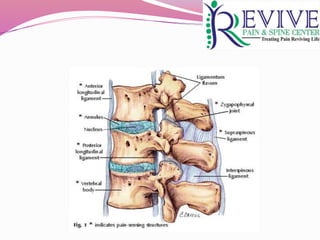
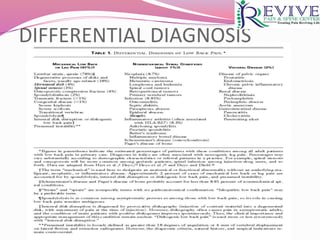
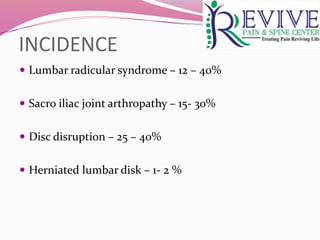
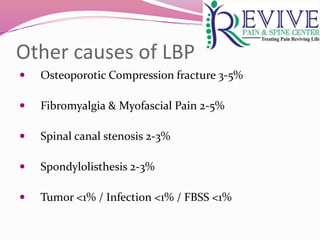
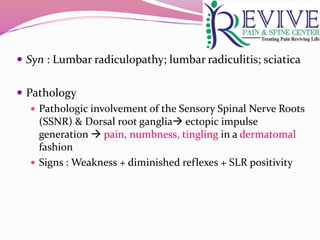
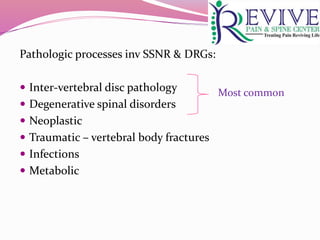
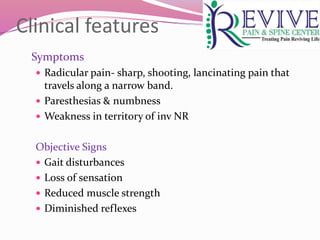
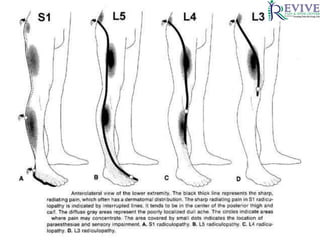
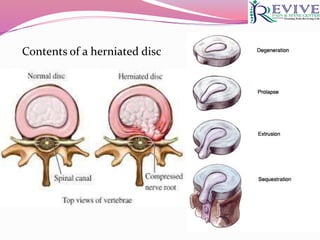
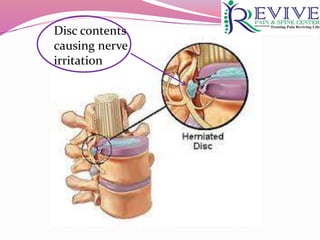
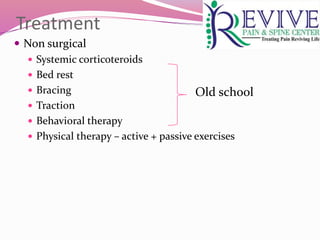
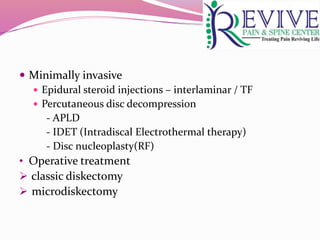
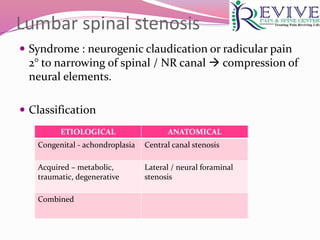
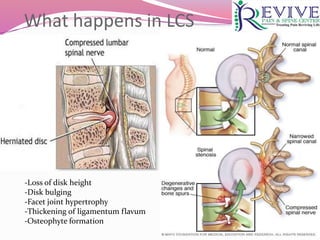
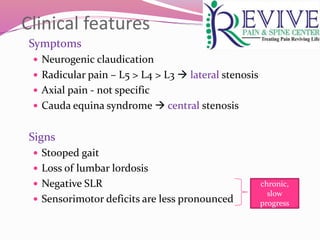
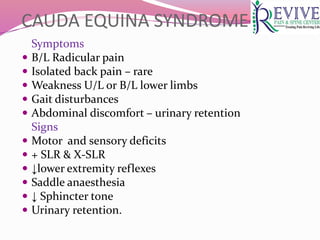
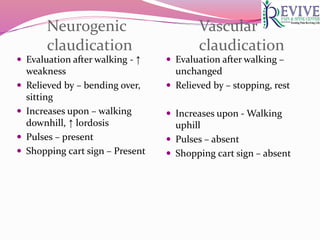
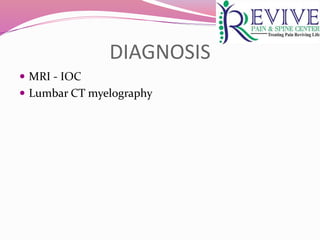
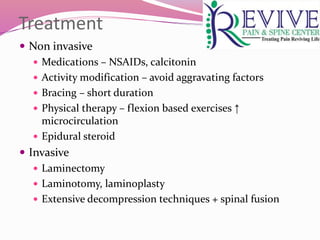
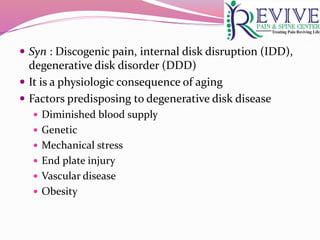
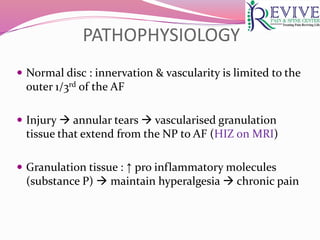
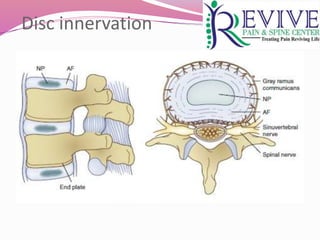
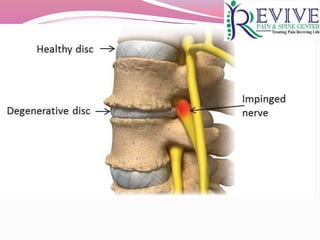
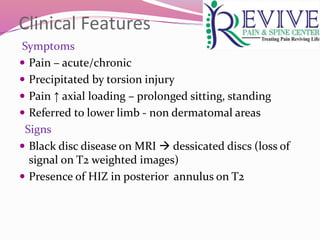
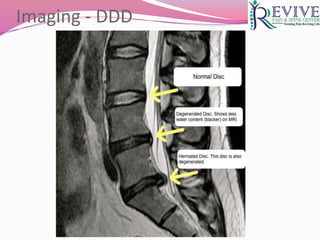
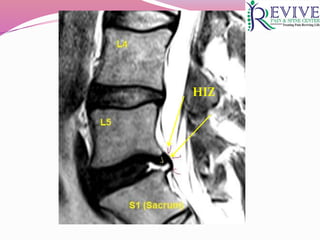
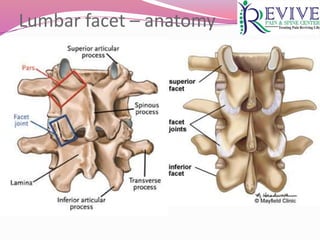
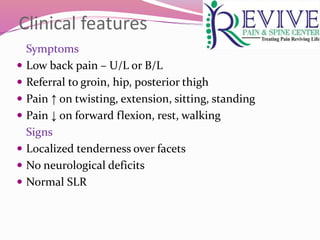
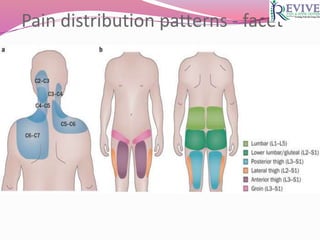
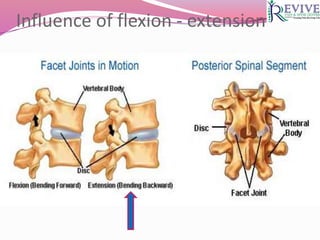
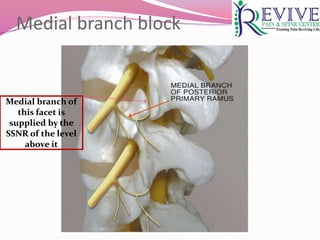
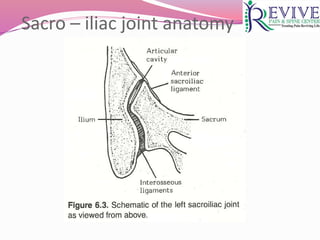
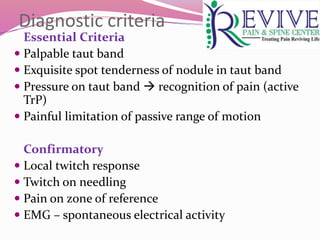
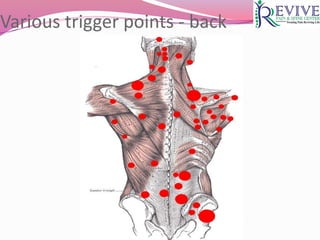
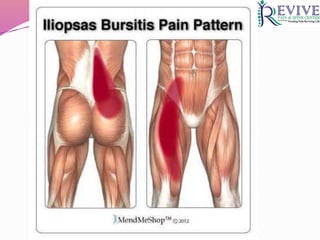
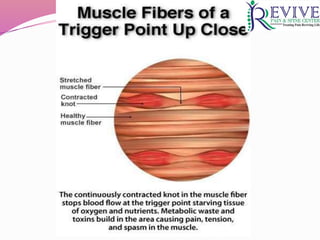
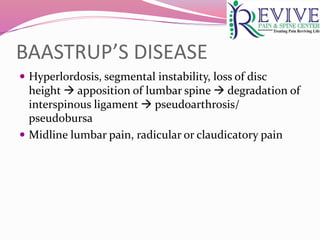
This document provides an overview of low back pain (LBP) by Dr. Varun Singla. It discusses the incidence and sources of LBP, including vertebral bodies, discs, facet joints, spinal nerves, muscles and ligaments. Differential diagnoses covered include lumbar radiculopathy, disc disorders, spinal stenosis, sacroiliac joint dysfunction and myofascial pain. Diagnostic tests and treatment approaches are described for each condition. Imaging findings and pathophysiology of herniated discs are detailed. Facet joint anatomy and causes of facet syndrome are reviewed.