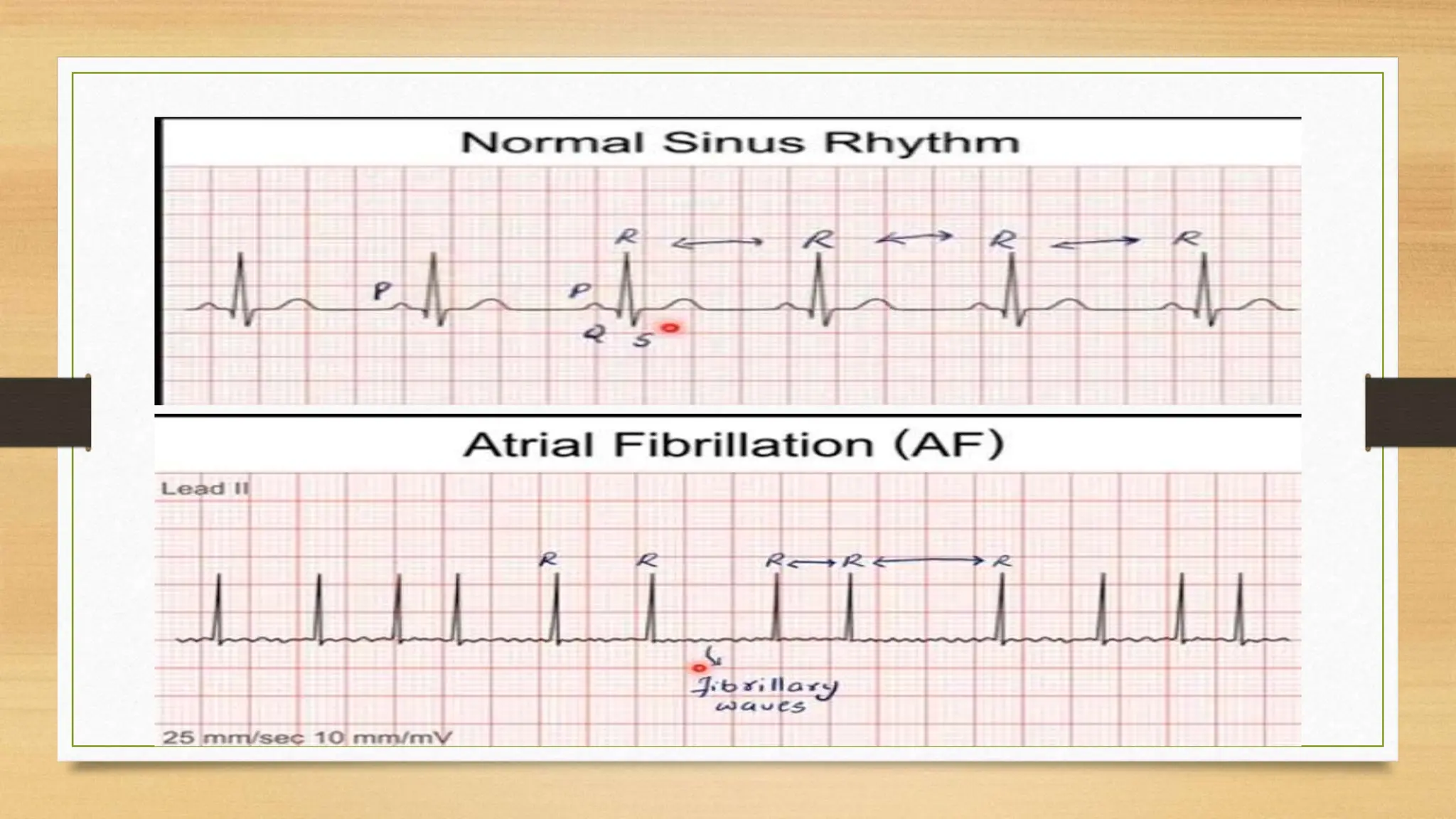
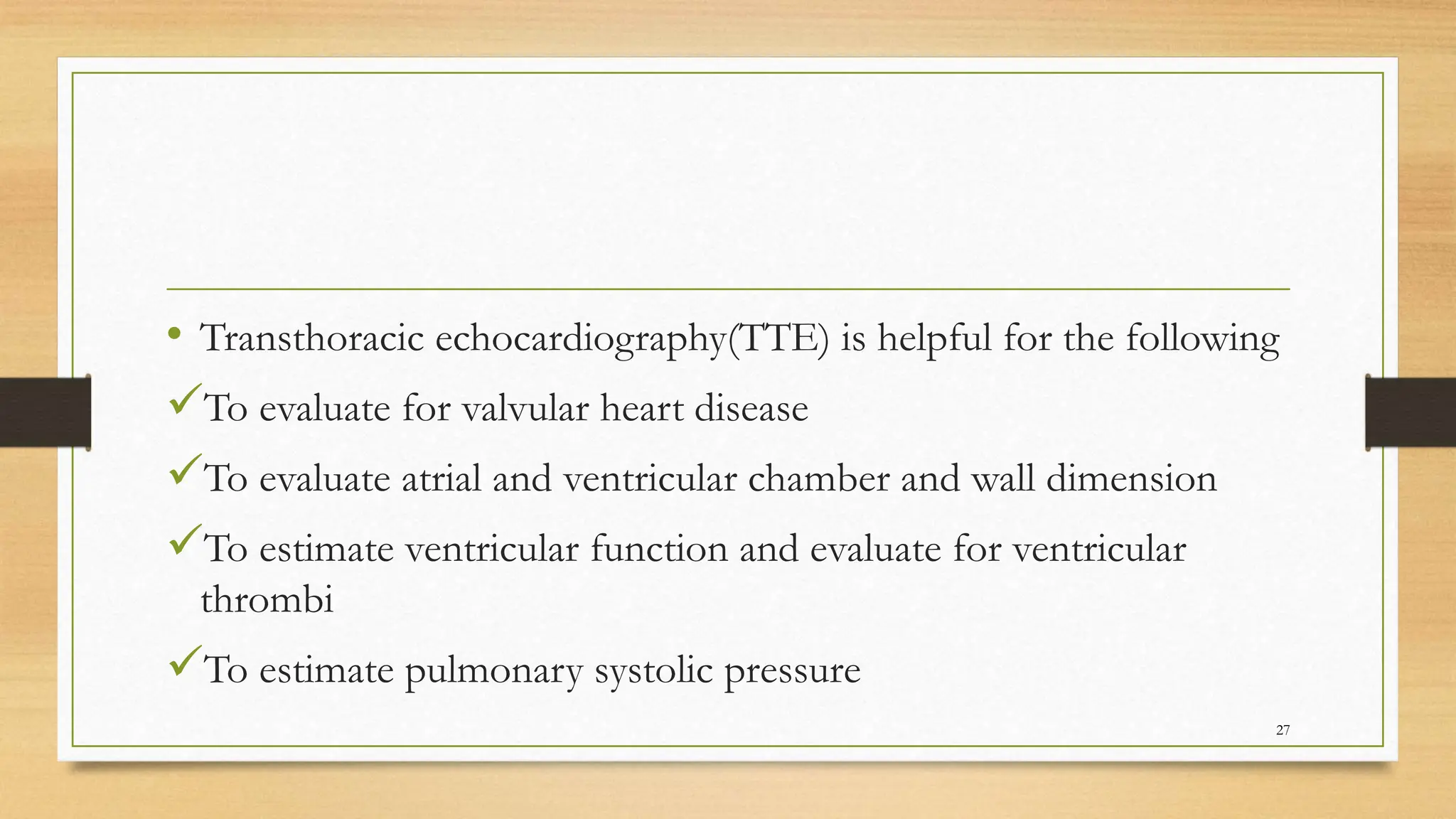
The document provides a comprehensive overview of atrial fibrillation (AF), detailing its epidemiology, etiology, clinical presentation, diagnosis, and management strategies. AF is characterized as a common cardiac arrhythmia with significant risks, especially among older populations, and requires careful assessment and a multidisciplinary approach for effective management. Key management strategies include pharmacological interventions, lifestyle modifications, and consideration of thromboembolic risks using scoring systems.













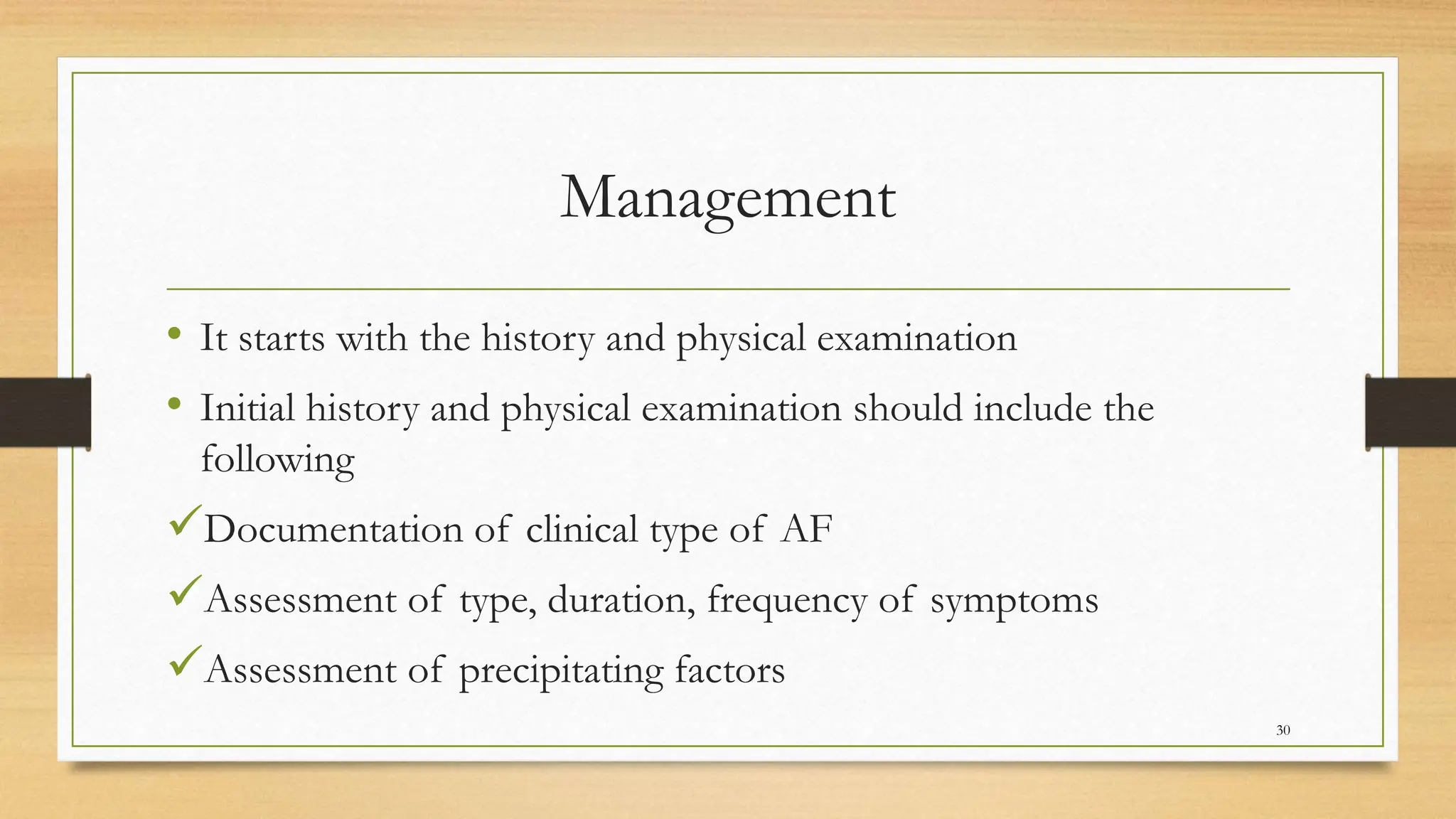









![CHA2 DS2-VASc Score Recommended Therapy
0 No therapy
1
No therapy, or aspirin 81-325 mg daily, or
anticoagulation therapy
(eg, warfarin [international normalized ratio
(INR) goal 2-3], dabigatran, rivaroxaban,
apixaban, edoxaban)
≥2
Anticoagulation therapy (eg, warfarin [INR goal
2-3], dabigatran, rivaroxaban, apixaban,
edoxaban)
47](https://image.slidesharecdn.com/atrialfibrillationsautosavededited-231206202916-9b343305/75/Atrial-Fibrillations-47-2048.jpg)