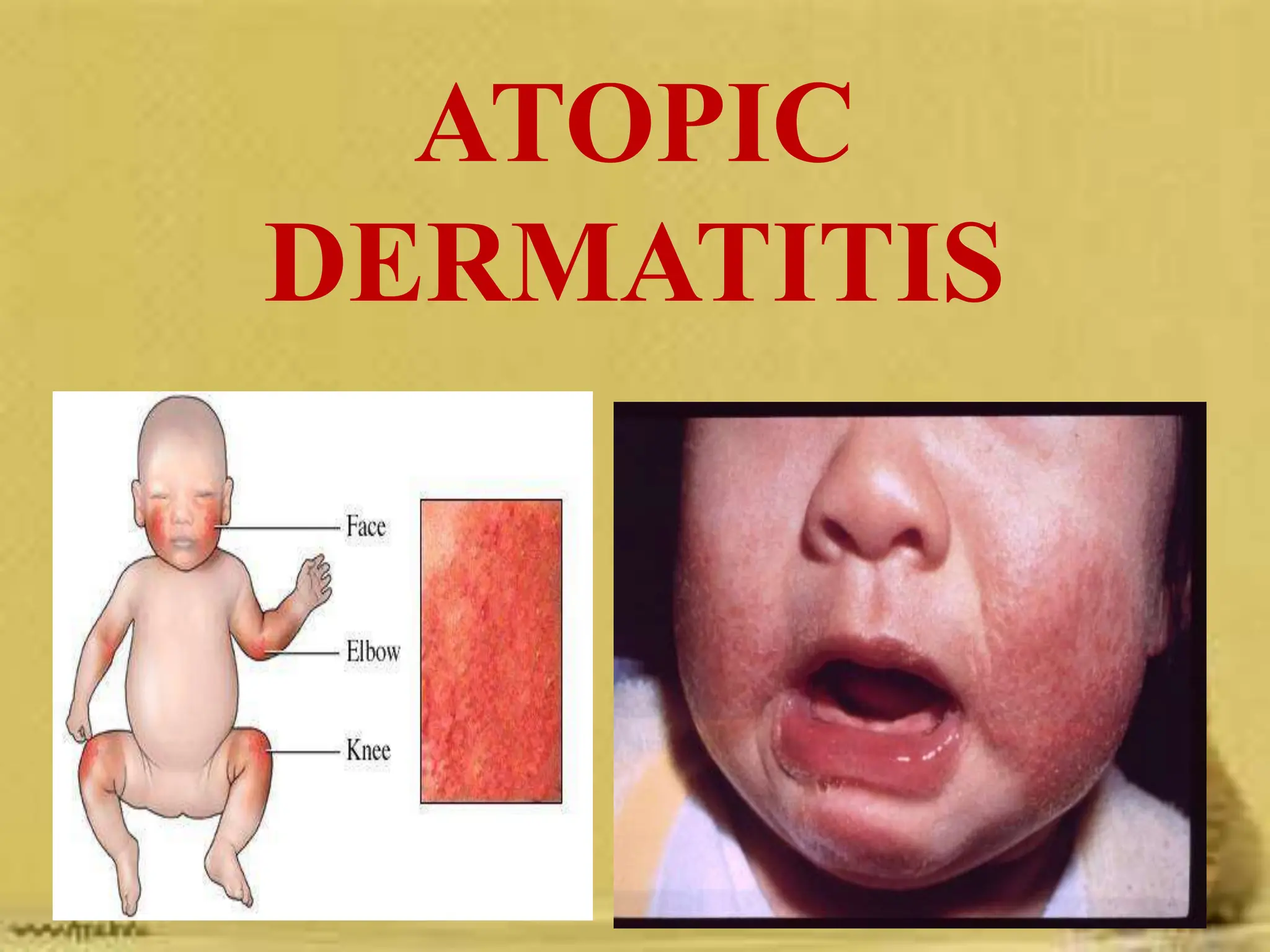
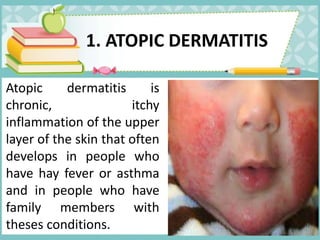
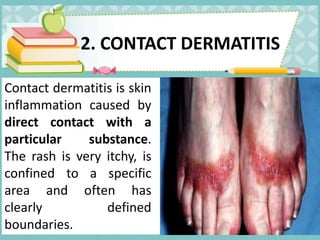
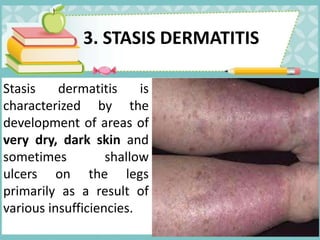
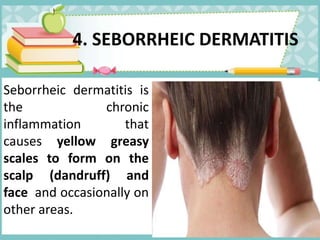
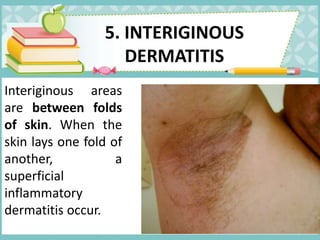
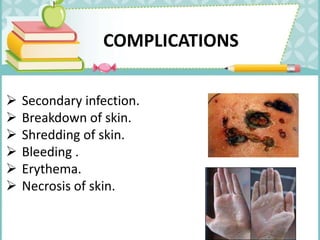
Atopic dermatitis is a chronic inflammatory skin condition characterized by itching, redness, and scaling, often linked to allergies and genetics. Various types of dermatitis include contact, stasis, seborrheic, and interiginous, each with specific causes and symptoms. Management includes medical and pharmacological treatments, nursing interventions, and education on hygiene and prevention of infections.