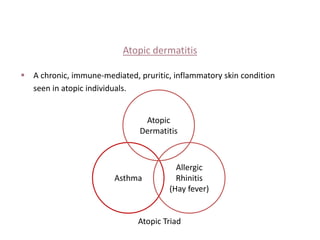
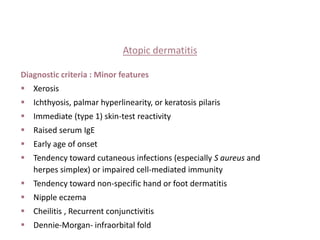
Atopic dermatitis is a chronic, pruritic inflammatory skin condition seen in individuals with a personal or family history of atopy. It is characterized by periods of flare-ups and remission influenced by environmental and emotional factors. The diagnosis is based on clinical features including pruritus, typical morphology and distribution of lesions, and a history of atopy. Management involves identifying triggering factors, using topical emollients and corticosteroids, oral antihistamines and antibiotics, and more intensive therapies for severe cases such as phototherapy or immunosuppressants.