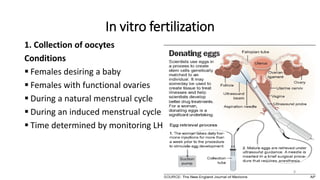
The document discusses assisted reproductive technology (ART), focusing on in vitro fertilization (IVF) and other methods for addressing infertility. It also highlights ethical issues surrounding ART, including complications from laboratory errors, donor anonymity, and the implications of surrogacy. The advancements in ART have brought about social, legal, and ethical challenges that need to be addressed as techniques evolve.