This document provides information on male infertility including:
- Common causes of male infertility include abnormal semen profile, sexual dysfunction, genetic factors, infections, etc.
- Evaluation of male infertility involves history, physical exam, semen analysis, and additional tests like hormone assays, immunological tests, and genetic analysis.
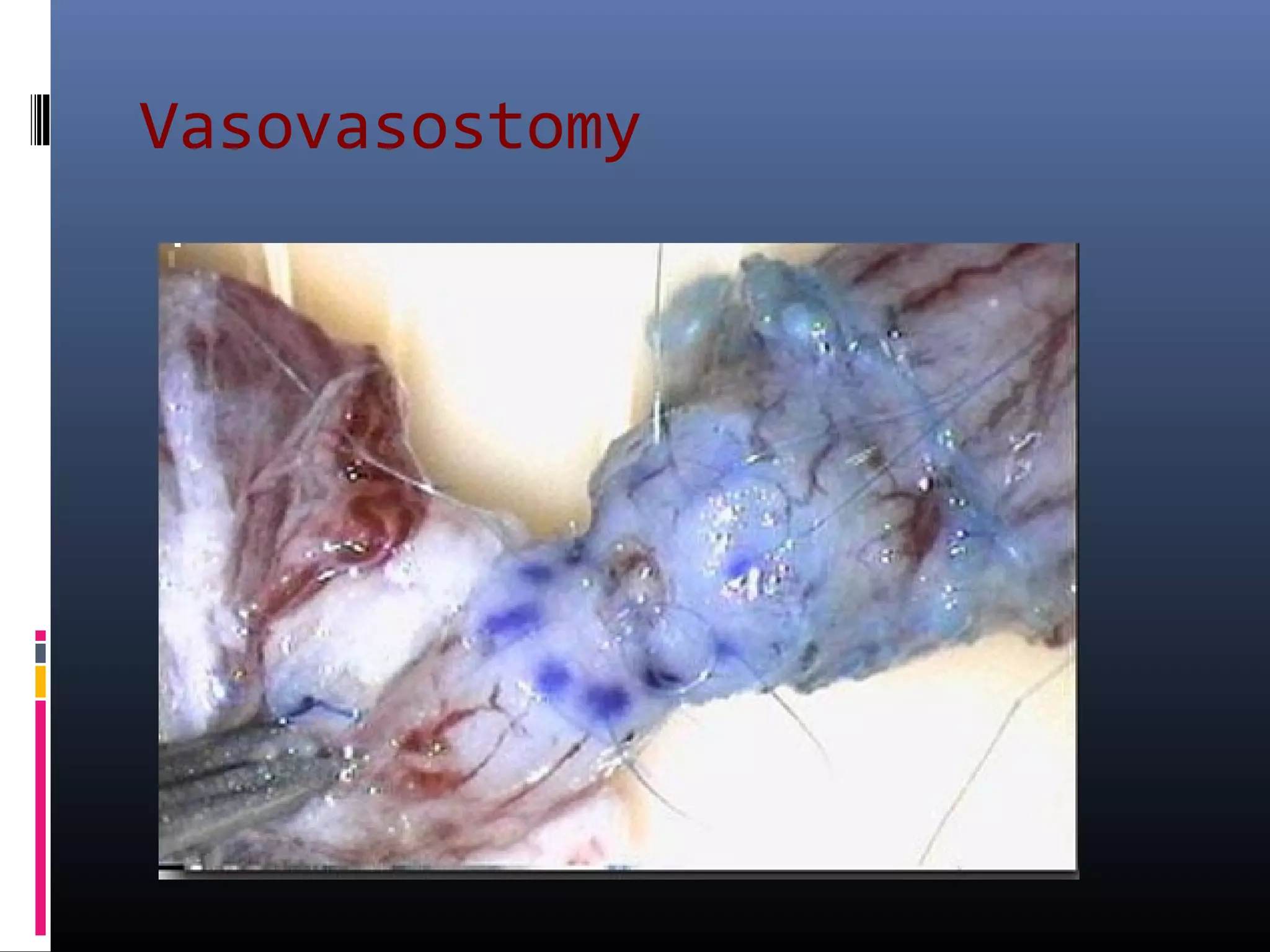
- Treatment depends on the underlying cause but may include lifestyle changes, medications, surgery, assisted reproductive technologies like IVF/ICSI.