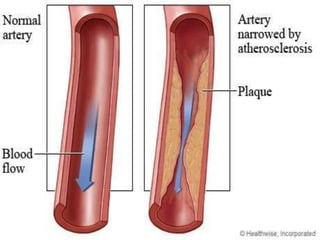
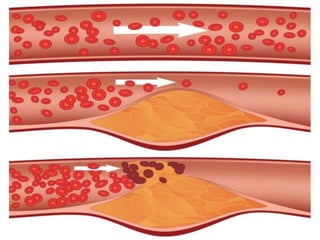
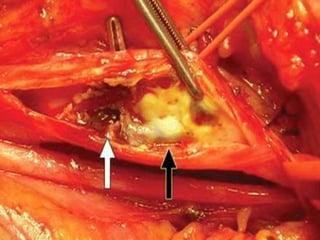
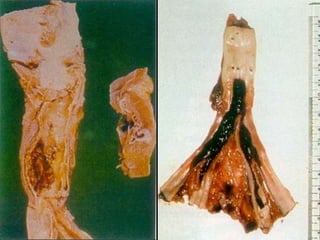
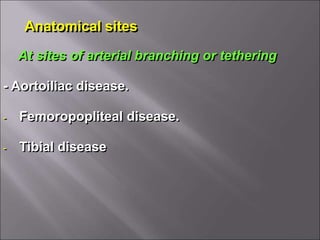
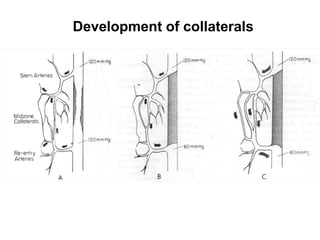
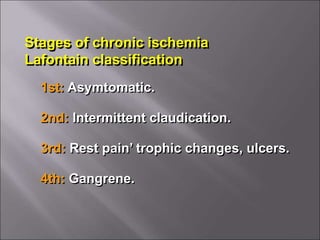
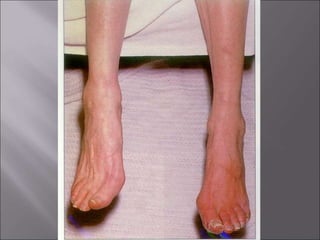
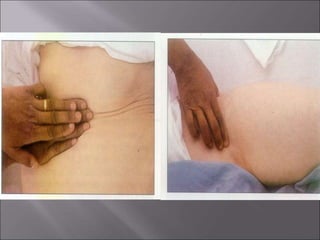
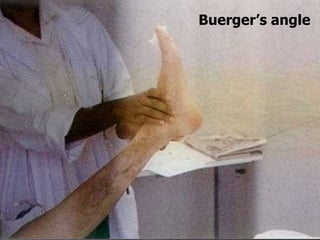
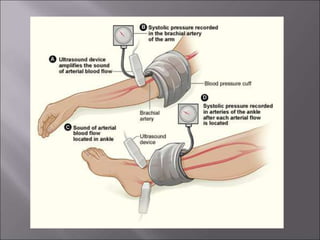
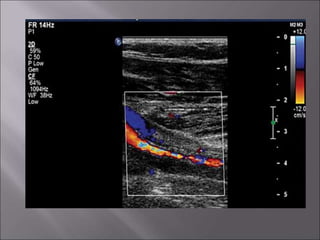
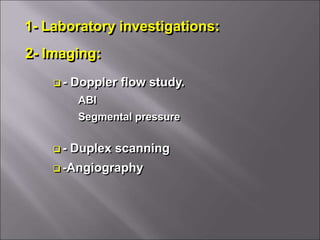
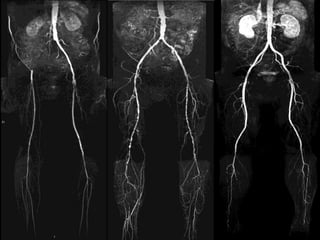
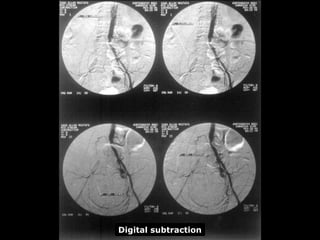
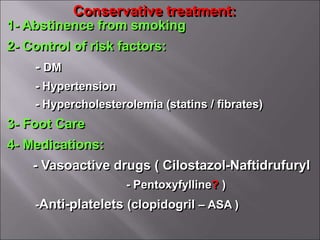
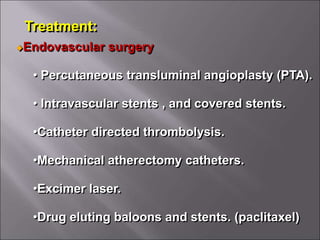
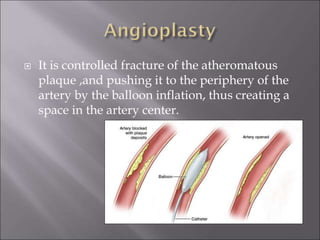
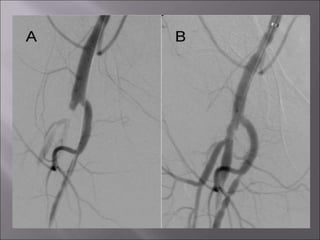
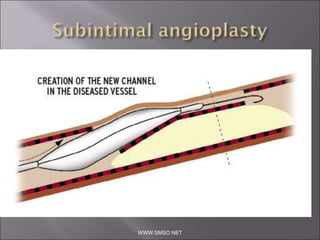
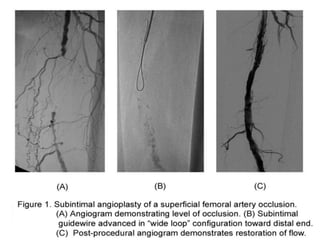
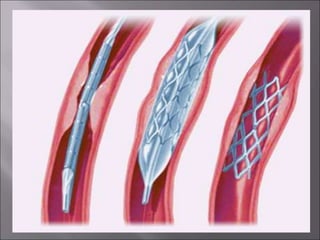
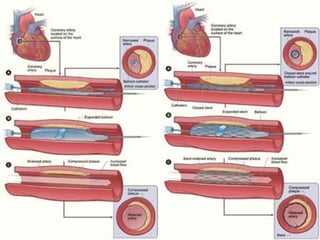
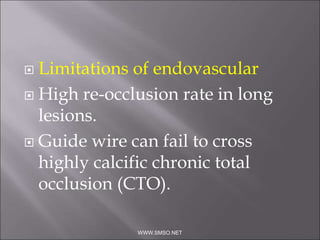
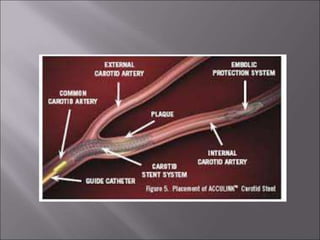
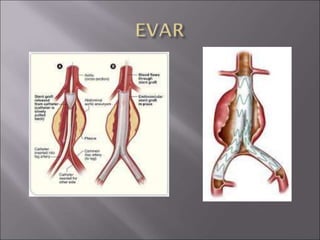
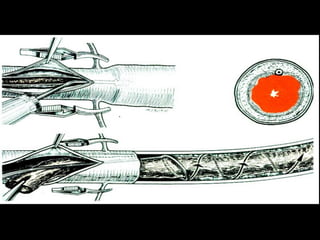
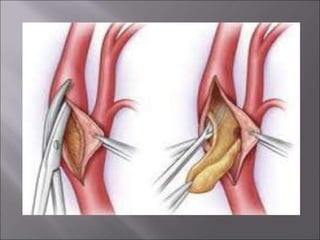
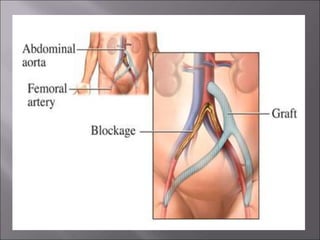
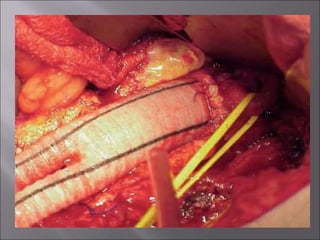
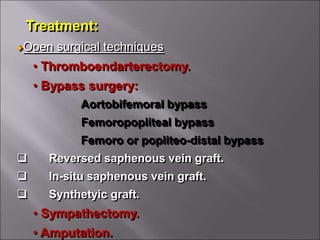
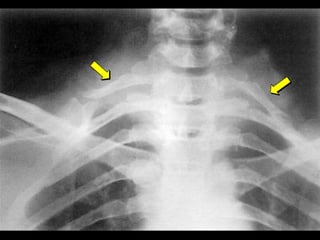
This document defines peripheral artery disease and describes its causes and presentation. PAD is caused by a reduction of blood flow in the arteries due to stenosis or occlusion. Major causes include atherosclerosis, Buerger's disease, vasospastic disorders like Raynaud's, and vasculitis. Clinical features include trophic skin changes, absent pulses, and symptoms ranging from intermittent claudication to critical limb ischemia. Diagnosis involves imaging like Doppler and angiography. Treatment options include conservative management, endovascular procedures like angioplasty, and open surgeries like bypass grafts and amputation.